Providing cancer immunotherapies with a boost could reduce cancer recurrence
Posted: 16 July 2020 | Hannah Balfour (Drug Target Review) | No comments yet
Researchers reveal drugs inhibiting Neuropilin-1 (NRP1), a protein expressed on T cells, could improve the efficacy of immunotherapies.
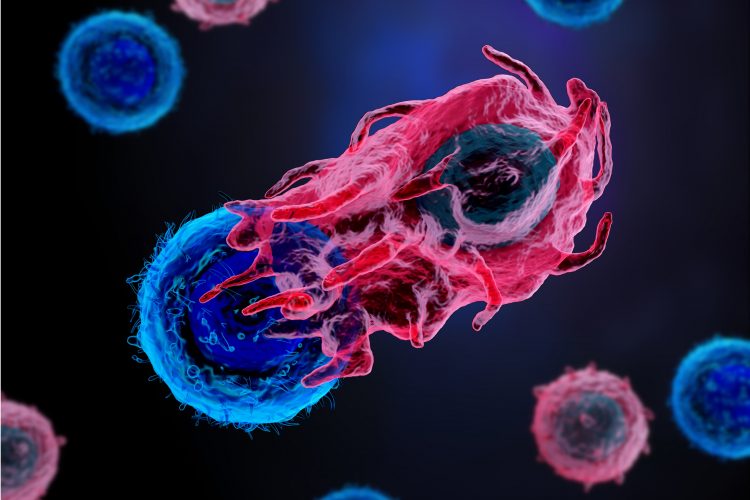
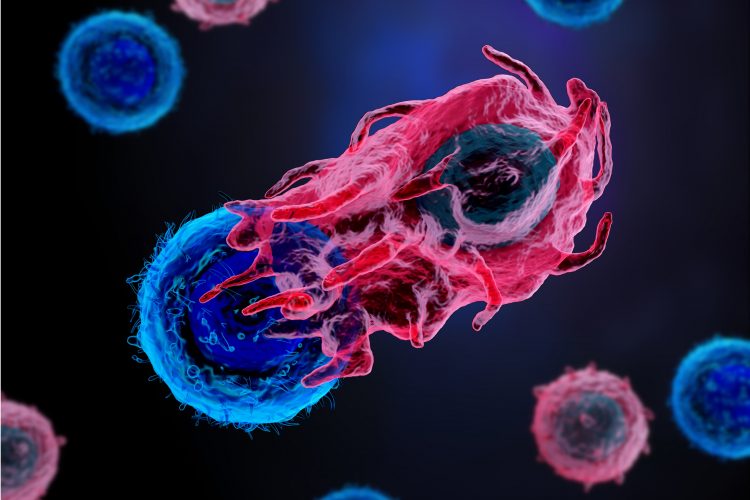
According to researchers, blocking an “immune memory checkpoint” on immune cells could improve immunotherapies and reduce cancer recurrence.
Blocking a newly identified “immune memory checkpoint” in immune cells could improve immunotherapy and help prevent cancers from recurring, according to new findings in mice and human samples by researchers at the UPMC Hillman Cancer Center and the University of Pittsburgh School of Medicine, both US.
The research published in Nature Immunology, suggests that by blocking Neuropilin-1 (NRP1), a protein on the surface of killer T cells which suppresses the immune response to cancer, immunotherapy drugs such as PD1 inhibitors may be made more effective across a wider range of patients.
“There is still much work to be done to improve cancer immunotherapy because only a small group of people benefit, and even among those, we see many tumours relapsing,” said Dr Dario Vignali, who holds the Frank Dixon Chair in Cancer Immunology at University of Pittsburgh’s School of Medicine and is the co-leader of the Cancer Immunology and Immunotherapy program at the UPMC Hillman Cancer Center. “Our findings point to an important new biological anti-tumour mechanism that we can exploit to provide durable, long-term immune response against tumours.”
Dr Chang “Gracie” Liu, a postdoctoral researcher in Vignali’s lab and first author of the publication explained, that they knew NRP1 was expressed on the surface of different T cells, but wondered whether it could alter the function of killer T cells. “We thought it might function like any other immune checkpoint molecule and that blocking it would prevent tumours from growing,” she said.
However, when Liu and colleagues grafted tumour cells into a genetically modified mouse that had NRP1 removed specifically from the surface of only killer T cells, they saw no difference at all in the speed or growth of the tumour.
“We were a bit disappointed and thought we had hit a dead end because it looked like removing NRP1 did not impact anti-tumour immunity,” she commented. “But instead of giving up, we asked a different question – does NRP1 change the capability of the immune system to remember the tumour?”
The team removed the tumour, waited and then grafted cancer cells into a different location in the mouse model. According to the scientists, what they observed was quite dramatic; mice that had NRP1 genetically deleted on killer T cells were better protected against the secondary tumour and responded more positively to anti-PD1 immunotherapy when compared to normal mice.
Further experiments revealed that NRP1 was controlling the fate of how T cells develop and establish immune memory – having NRP1 caused the killer T cells to become exhausted and ineffective in fighting cancer cells, particularly over the long-term, while removing NRP1 resulted in T cells having an increased immune memory.
According to the researchers, their finding correlates with studies of T cells isolated from patients with skin or head and neck cancers. Patients with advanced stage head and neck cancer had higher levels of NRP1 on a subset of memory killer T cells. In patients with advanced skin cancer treated with various immunotherapies, higher NRP1 levels on killer T cells were associated with a poorer response to treatment and a smaller pool of memory T cells.
“This is a completely new area of understanding of how anti-tumor immunity is controlled and will present new therapeutic opportunities to promote and enhance a more durable, long-term anti-tumour response in cancer patients,” said Vignali.
He continued that some drugs targeting NRP1 are already being tested in clinical trials in combination with anti-PD1 immunotherapies and hopes these will reveal more about the role of immune memory in fighting cancer.
Related topics
Disease research, Drug Targets, Immunooncology, Immunotherapy, In Vivo, Oncology, Protein Expression, Proteomics, Therapeutics
Related conditions
Cancer, Head and Neck cancer, Skin cancer
Related organisations
University of Pittsburgh School of Medicine, UPMC Hillman Cancer Center
Related people
Dr Chang "Gracie" Liu, Dr Dario Vignali


