Experimental CAR T therapy targets solid tumour cancer cells
Posted: 3 July 2020 | Hannah Balfour (Drug Target Review) | No comments yet
Scientists have developed a novel chimeric antigen receptor (CAR) T-cell therapy to target a variety of human and murine solid-tumour cancer cells.
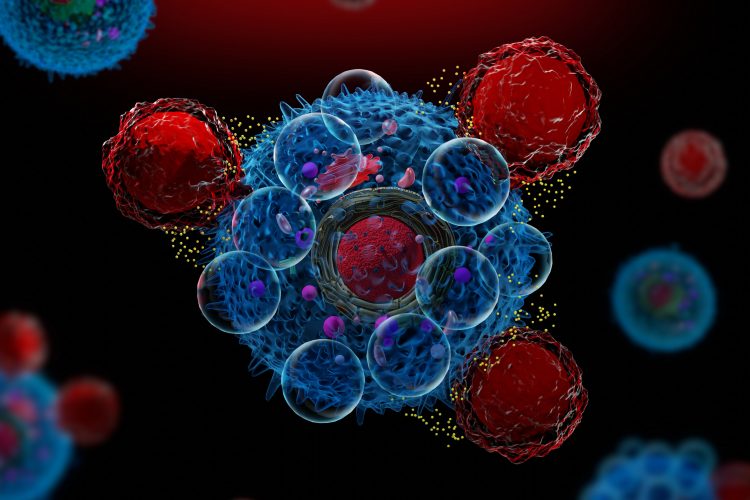
Chimeric antigen receptor (CAR) T-cell therapies have been highly successful in patients with blood cancers such as lymphoma and leukaemia; however, targeting them specifically to solid tumours has not been fruitful so far. “A major challenge in the field has been to identify targets that exist on cancer cells in solid tumours that are not present on normal tissue,” said David Kranz, research co-leader, biochemistry professor at the University of Illinois and a member of the Cancer Center at Illinois.
In a study published in the PNAS researchers modified T cells with an antibody fragment targeting proteins bound to an abnormal length of sugar chain that appear on the surface of several solid tumour types. These abnormally short sugar chains on some types of cancer cells result from mutations that disrupt the molecular pathway that attaches them to proteins, said Preeti Sharma, a postdoctoral researcher at the University of Illinois at Urbana-Champaign who also led the research. Drugs that bind to these aberrant sugars preferentially recognise cancer cells and spare healthy cells.
The team started their design with a piece of an antibody known to interact with a specific type of abnormally formed sugar attached to a protein on solid-tumour cancer cells in mice.
“We realised that because this receptor binds both to the protein and the sugar on the surface of the cancer cell, there might be room to change the antibody so that it can bind to more than one protein attached to the short sugar,” Sharma said. “This could make it broadly reactive to different kinds of cancers.”
Study co-author Qi Cai (postdoctoral researcher in the Kranz lab) experimented with alterations to the sequence of the amino acids in the vicinity of the abnormal sugar to assess whether this affected the ability of the receptor to bind at the site. The team determined that, if the antibody could be slightly changed, it potentially could accommodate other sugar-linked cancer targets.
Sharma said they then conducted a series of mutation experiments focused on the essential parts of the antibody: “We generated almost 10 million mutant versions of our receptor, and then we screened those to find the property we wanted. In this case, we wanted to broaden the specificity of that antibody so that it reacts not only to the mouse target but also to human targets.”
Once antibodies with this trait were identified, the team engineered them into T cells and tested them on human and murine cancer cell lines. The CAR T cells showed activity against cell lines from both species. Sharma added: “… the T-cells can now recognise several different proteins that have short sugars attached to them. This is really important because in cancer therapy, most of the time you are going after a single target on a cancer cell. Having multiple targets makes it very difficult for the cancer to evade the treatment.”
Kranz concluded: “Although these engineered cells are early in development, we are particularly excited that we can use the same T-cell product to study efficacy and safety against cancers in mice and humans.”
Related topics
Antibodies, Chimeric antigen receptors (CARs), Drug Development, Drug Targets, Immunooncology, Immunotherapy, Proteomics, Research & Development, t-cells, Therapeutics
Related conditions
Leukaemia, lymphoma, Solid tumour cancer
Related organisations
University of Illinois at Urbana-Champaign
Related people
David Kranz, Preeti Sharma, Qi Cai



