High-throughput screening reveals new compound to maintain lung health
Posted: 21 February 2020 | Victoria Rees (Drug Target Review) | No comments yet
Researchers have screened 20,000 molecules to discover a potent compound with low toxicity that restores the balance of healthy stem cells in the lungs of mice.
A molecule identified by researchers through screening helps maintain a healthy balance of cells in airway and lung tissue. According to the scientists, if the compound, so far only studied in isolated human and mouse cells, has the same effect in people, it may lead to new drugs to treat or prevent lung cancer.
“We think this could help us develop a new therapy that promotes airway health,” said Dr Brigitte Gomperts, lead author of the study and professor of paediatrics and pulmonary medicine at the University of California LA (UCLA), US, where the stiudy was conducted. “This could not only inform the treatment of lung cancer, but help prevent its progression in the first place.”
The human respiratory system is regularly replenished with healthy cells. That process is driven by airway basal stem cells, which divide to produce both more stem cells and the mucociliary cells that line the airways and lungs.
Mucociliary cells include:
- mucus cells, which produce the mucus that trap toxic and infectious particles
- ciliated cells, which have finger-like projections that sweep the mucus away to keep the respiratory system healthy and clear.
In healthy lungs, airway basal stem cells stay balanced between producing mucociliary cells and self-renewing to maintain a population of stem cells. In pre-cancerous cells in the lungs, basal stem cells divide more often than usual, generating a large number of stem cells but too few mucociliary cells. The resulting imbalance of cells in the airway leaves it unable to properly clear debris and creates a greater risk that the pre-cancerous cells will develop into a tumour.
In the new study, the researchers analysed airway cells from equal numbers of biopsies of healthy people, patients with pre-malignant lung cancer lesions and patients with squamous lung cancer. They discovered that one group of molecules – collectively called the Wnt/beta-catenin signaling pathway – was present at different levels in the basal stem cells of the patient samples versus the cells from healthy people.
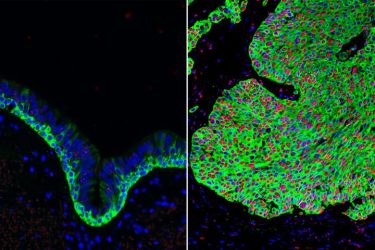
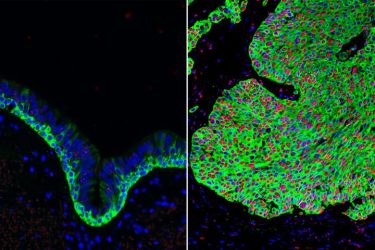
Normal airway tissue, left and lung cancer tissue, right, with an overabundance of basal stem cells (green). The activated form of beta-catenin (red) in the lung cancer can be targeted by the Wnt Inhibitor Compound 1 (credit: Broad Stem Cell Research Center).
Altering the levels of these molecules in healthy airway cells from mice, the team found the balance between stem cells and mucociliary cells shifted, mimicking the imbalance seen in lung pre-cancers.
“When you activate the Wnt/beta-catenin signaling pathway, these stem cells just divide and divide,” said Gomperts.
Finally, the researchers screened more than 20,000 chemical compounds using high-throughput methods. They investigated their ability to reverse this effect in human cells, lowering levels of Wnt and restoring the balance of stem cells and mature airway cells.
One compound, named as Wnt Inhibitor Compound 1 (WIC1), was particularly effective at limiting the proliferation of basal stem cells and restoring the balance of the stem cells and mucociliary cells to regular levels. The researchers also noted that the compound was less toxic to airway cells than previously discovered molecules that block Wnt/beta-catenin signalling.
“The identification of this new drug is a nice tool to tease apart the biology of the Wnt/beta-catenin signalling pathway and its effects on lung health,” said Cody Aros, the first author of the new paper and a UCLA graduate student. “It’s also very exciting that it may act in a new way than other existing Wnt/beta-catenin signalling pathway inhibitors and has such low toxicity.”
As WIC1 was identified through a random drug screen, the researchers do not yet know exactly how it works, but they are planning future studies on its mechanism and safety.
The study was published in Cell Reports.
Related topics
Drug Targets, High Throughput Screening (HTS), Molecular Targets, Screening, Stem Cells
Related conditions
Lung cancer
Related organisations
University of California LA (UCLA)
Related people
Cody Aros, Dr Brigitte Gomperts


