New study reveals causes of stem cell transplant rejection
Posted: 20 August 2019 | Rachael Harper (Drug Target Review) | No comments yet
A new study has shown that mutations in mitochondrial DNA induced by cell reprogramming may trigger an immune response.
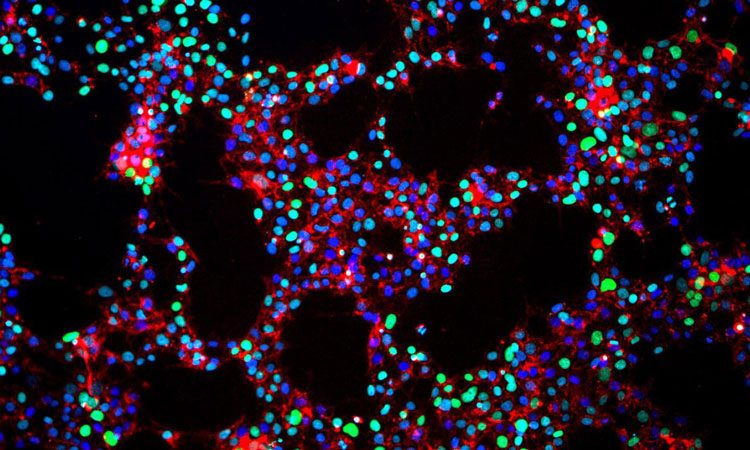
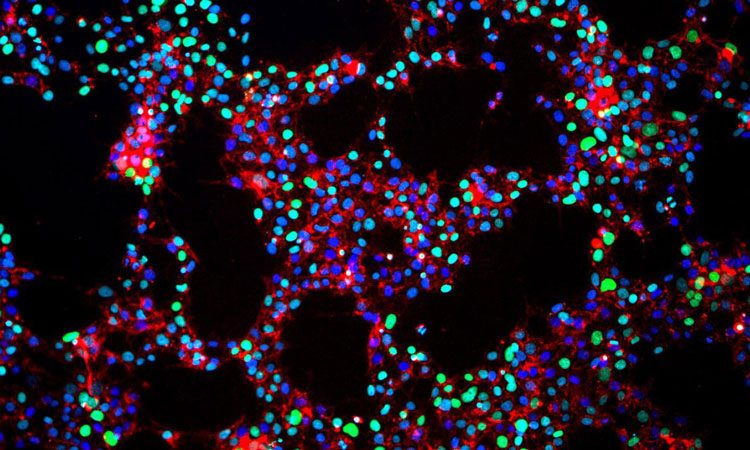
Image credit: UCSF
A new study from the UC San Francisco Transplant and Stem Cell Immunobiology (TSI) Lab, in collaboration with the Laboratory of Transplantation Genomics at the National Heart, Lung, and Blood Institute (NHLBI) and Stanford University, has shown that the adult-to-induced pluripotent stem cells (iPSC) conversion process can mutate DNA found in tiny cellular structures called mitochondria.
These mutations can then trigger an immune response that causes mice and humans to reject iPSCs and stem cell transplants more generally.
The human mitochondrial genome contains only 13 protein-coding genes and fewer than 17,000 bases. However, in tissues with high energy demands, the tiny mitochondrial genome can contribute disproportionately to cells’ total protein content.
“In cells that do a lot of work, like heart muscle cells, up to a third of the cell’s protein-producing mRNA molecules are mitochondrial in origin,” said Sonja Schrepfer, MD, PhD, professor of surgery and senior author of the study.
“This means that the burden of a single mitochondrial mutation may be tremendous. You don’t end up with just a few proteins that can potentially provoke an immune response – you end up with thousands.”
To show that such mitochondrial mutations can trigger an immune response, the scientists created hybrid stem cells with nuclear DNA from one mouse strain and mitochondrial DNA from another. They transplanted these cells into mice with identical nuclear DNA, but whose mitochondrial DNA differed by a single base in two protein-coding genes. A few days post-transplant, they harvested immune cells from the mice and exposed the cells to various mitochondrial protein fragments. The only proteins that triggered a response were those produced by the two ‘foreign’ mitochondrial genes.
To perform these experiments in humans, the researchers “recruited liver and kidney transplant patients and designed experiments that took advantage of naturally occurring sequence differences in the mitochondrial DNA of donors and recipients,” said Tobias Deuse, MD, the lead author of the study.
As in the mouse experiments, the researchers isolated immune cells from each transplant recipient and exposed the cells to mitochondrial protein fragments. The results were identical: the recipient’s immune cells were only triggered by the ‘foreign’ mitochondrial proteins that originated from the organ donor.
“In both mouse and human, even one mitochondrial mutation is enough to have a recognisable immune response,” Schrepfer added.


Tobias Deuse, MD, lead author and Sonja Schrepfer, MD, PhD, senior author of the study (credit: UCSF).
The iPSC conversion process is highly mutagenic and gives rise to many new, immune-activating mitochondrial mutations, said Deuse. “Under normal physiological conditions, mitochondrial DNA is 10 to 20 times more susceptible to mutation than nuclear DNA. Transforming adult cells into stem cells is a harsh process, so we expected mutation rates to be just as high or higher.”
Mitochondria also lacks the molecular machinery that repairs DNA. Instead, the body relies on the immune system to find and destroy cells that produce unfamiliar mitochondrial proteins – a clear sign that the mitochondrial DNA has mutated. But cells that become iPSCs are reprogrammed and grown outside of the body and do not undergo this weeding out process by the immune system, Shrepfer said.
However, Deuse and Schrepfer say that: “The bottom line is that we want to make people aware of this phenomenon. Just because iPSCs are derived from your own cells doesn’t necessarily mean they won’t induce an immune response. It’s very easy to introduce mutations during iPSC production, so it’s critical that iPSC and stem cell products used therapeutically are screened for mitochondrial mutations prior to transplant.”
The study was published in Nature Biotechnology.
Related topics
Analysis, DNA, Immunology, miRNAs, Regenerative Medicine, Research & Development, Stem Cells
Related organisations
National Heart Lung and Blood Institute (NHLBI), Nature Biotechnology, Stanford University, UC San Francisco (UCSF)
Related people
Professor Sonja Schrepfer, Tobias Deuse


