3D liver tissue made from stem cells show promising support of liver function
Posted: 5 September 2018 | Drug Target Review | No comments yet
Stem cells transformed into 3D human liver tissue by scientists show promising support of liver function when implanted into mice with a liver disease…
Stem cells transformed into 3D human liver tissue by scientists from the MRC Centre for Regenerative Medicine at the University of Edinburgh show promising support of liver function when implanted into mice with a liver disease.
The scientists say that in addition to being early-stage progress towards developing human liver tissue implants, it could also reduce the need for animals in research by providing a better platform to study human liver disease and test drugs in the lab.
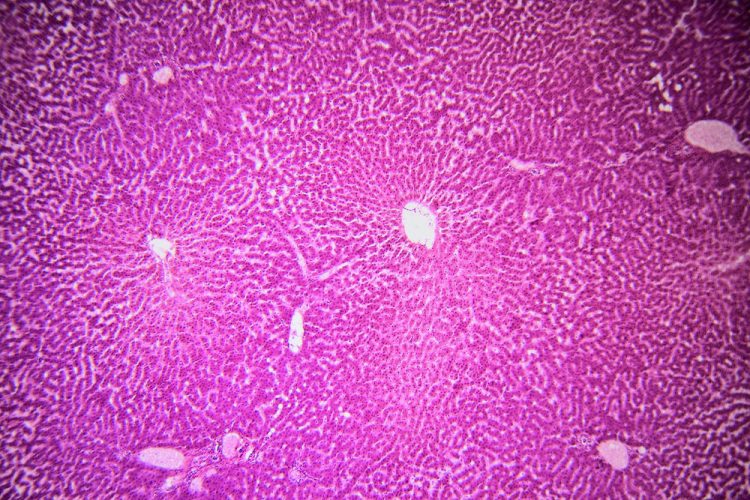
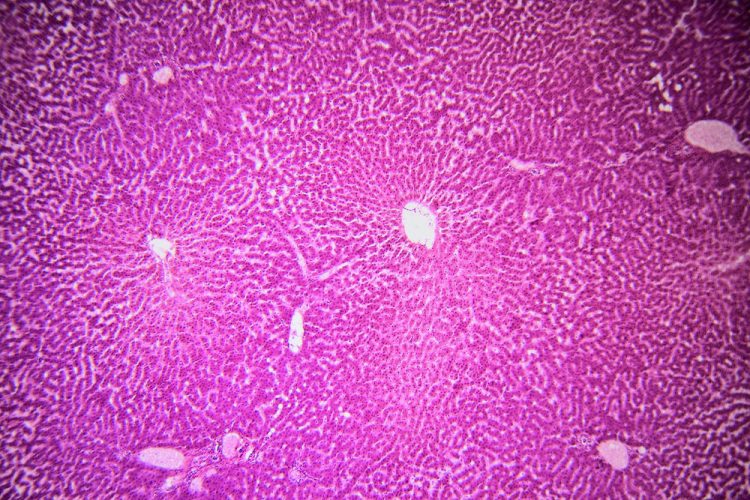
The scientists took human embryonic stem cells and induced pluripotent stem cells and carefully stimulated them to develop the characteristics of liver cells, called hepatocytes. They grew these cells as small spheres in a dish for over a year.
Professor David Hay from the MRC Centre for Regenerative Medicine at the University of Edinburgh, who led the research, said: “This is the first time anyone has kept stem cell-derived liver tissue alive for more than a year in the lab. Keeping the cells alive and stable as liver cells for a long time is a very difficult step, but crucial if we hope to use this technology in people.”
The scientists then collaborated with materials chemists and engineers to identify suitable polymers already approved for use in humans in order to develop them into 3D scaffolds. The best material was a biodegradable polyester, polycaprolactone, which was spun into microscopic fibres. The fibre mesh formed a scaffold one-centimetre square and a few millimetres thick.
Liver cells derived from embryonic stem cells were loaded onto the scaffolds and implanted under the skin of mice.
Blood vessels successfully grew on the scaffolds and the mice were found to have human liver proteins in their blood, indicating that the tissue had successfully integrated with the circulatory system. The scaffolds were not rejected by the animals’ immune systems.
The liver tissue scaffolds were tested in mice with tyrosinaemia, a potentially fatal genetic disorder where the enzymes in the liver that break down the amino acid tyrosine are defective, resulting in the accumulation of toxic metabolic products.
The implanted liver tissue helped the mice with tyrosinaemia to break down tyrosine. Compared with mice in a control group that received empty scaffolds, the mice with liver implants lost less weight, had less accumulation of toxins in the blood, and showed fewer signs of liver damage.
Professor Hay said: “Bringing together biologists, chemists and engineers, helped us to develop our new polymer scaffolds for lab-grown liver cells and we’re excited that the implants successfully aided liver function. We hope implants like these may one day be able to help people with failing livers. Placing the scaffolds under the skin has the big advantage of being less invasive and potentially safer than inserting tissue grafts into the abdomen.
“Liver disease is a serious and increasing problem – it’s currently the fifth biggest killer in the UK – and many people with liver disease will die waiting for a transplant or develop complications from the immunosuppressive drugs after a transplant, so we urgently need to find alternatives. These results are an important early step and now we need to conduct longer-term studies to fully establish the safety of this technique and to scale up and optimise the performance of the liver tissue so we can move this technology towards clinical trials.”
Dr Rob Buckle, Chief Science Officer at the MRC, commented: “This research brings us a step closer to harnessing the potential of stem cell ‘reprogramming’ technologies to provide renewable supplies of liver tissue products for transplantation. Showing that such stem-cell derived tissue is able to reproduce aspects of liver function in the lab also offers real potential to improve the testing of new drugs where more accurate models of human tissue are needed.”
The study was funded by the UK Regenerative Medicine Platform (UK RMP) and the Chief Scientist Office Scotland. The UK RMP is a £42 million initiative by the Biotechnology and Biological Sciences Research Council, the Engineering and Physical Sciences Research Council and the MRC to ensure that research addressing regenerative medicine connects seamlessly from discovery science through to clinical and commercial application.
Read more about recent liver research from the MRC Centre for Regenerative Medicine: a study with mice found a class of drugs under development as a cancer treatment could help prompt the liver to regenerate after injury.
The study has been published in the journal Archives of Toxicology.
Related topics
Cell culture, Disease research, Induced pluripotent (iPS) cells, Research & Development, Stem Cells
Related conditions
Liver cancer, Liver disease
Related people
Dr Rob Buckle, Professor David Hay


