Astrocytes may help brain heal from stroke and spinal cord injuries
Posted: 30 March 2018 | Dr Zara Kassam (Drug Target Review) | No comments yet
Scientists have found a genetic trigger that may improve the brain’s ability to heal from a range of debilitating conditions…
Scientists have found a genetic trigger that may improve the brain’s ability to heal from a range of debilitating conditions, from strokes to concussions and spinal cord injuries.
A new study in mice from UT Southwestern’s O’Donnell Brain Institute shows that turning on a gene inside cells called astrocytes results in a smaller scar and – potentially – a more effective recovery from injury.
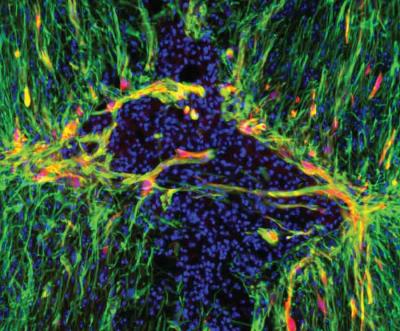
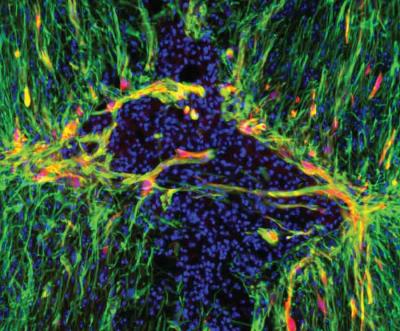
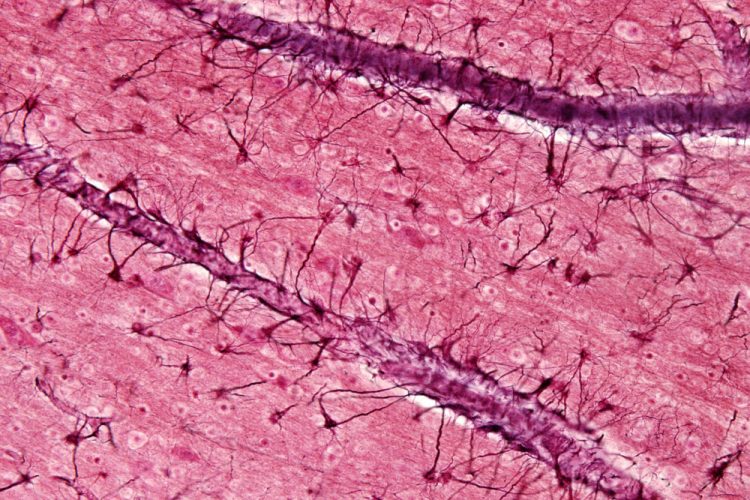
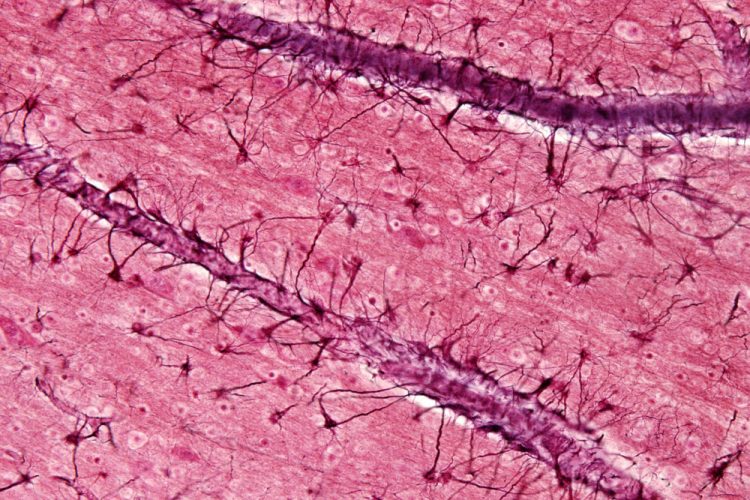
Genetically modified astrocytes (red) line the lesion border in the injured spinal cord. A new mouse study shows that triggering a gene inside astrocytes activates the star-shaped cells and may improve the brain’s ability to heal from a range of debilitating conditions, from stroke to concussions and spine injuries. Meifan Amy Chen, Ph.D. UT Southwestern
The research examined spinal injuries but likely has implications for treating a number of brain conditions through gene therapy targeting astrocytes, said Dr Mark Goldberg, Chairman of Neurology & Neurotherapeutics at UT Southwestern.
“We’ve known that astrocytes can help the brain and spinal cord recover from injury, but we didn’t fully understand the trigger that activates these cells,” Dr Goldberg said. “Now we’ll be able to look at whether turning on the switch we identified can help in the healing process.”
The study found that the LZK gene of astrocytes can be turned on to prompt a recovery response called astrogliosis, in which these star-shaped cells proliferate around injured neurons and form a scar.
Scientists deleted the LZK gene in astrocytes of one group of injured mice, which decreased the cells’ injury response and resulted in a larger wound on the spinal cord. They overexpressed the gene in other injured mice, which stimulated the cells’ injury response and resulted in a smaller scar. Overexpressing the gene in uninjured mice also activated the astrocytes, confirming LZK as a trigger for astrogliosis.
Dr Goldberg said a smaller scar likely aids the healing process by isolating the injured neurons, similar to how isolating a spreading infection can improve recovery. “But we don’t know under what circumstances this hypothesis is true because until now we didn’t have an easy way to turn the astrocyte reactivity on and off,” he said.
Further study is needed to analyse whether a compact scar tissue indeed improves recovery and how this process affects the neurons’ ability to reform connections with each other.
Dr Goldberg’s lab will conduct more research to examine the effects of astrogliosis in stroke and spinal cord injuries. The researchers will determine whether turning up LZK in mice in advance of an injury affects its severity. They will then measure how the formation of the compact scar helps or hinders recovery.
“It has been a big mystery whether increasing astrocyte reactivity would be beneficial,” said Dr Meifan Amy Chen, the study’s lead author and Instructor of Neurology at the Peter O’Donnell Jr Brain Institute. “The discovery of LZK as an on switch now offers a molecular tool to answer this question.”
The study has been published in Cell Reports
Related topics
Genomics
Related conditions
concussion, Stroke
Related organisations
UT Southwestern's O'Donnell Brain Institute
Related people
Dr Mark Goldberg, Dr Meifan Amy Chen, Peter O'Donnell Jr


