Targeting disease pathways to treat ulcerative colitis – beyond corticosteroid use
Posted: 29 September 2021 | Dr Chetan Karyekar (Janssen) | No comments yet
Dr Chetan Karyekar, Compound Development Team Leader at The Janssen Pharmaceutical Companies of Johnson & Johnson (J&J), explains how targeting underlying immune pathways can open the door to effectively treating more inflammatory bowel disease (IBD) patients by reducing or eliminating the chronic use of corticosteroids.
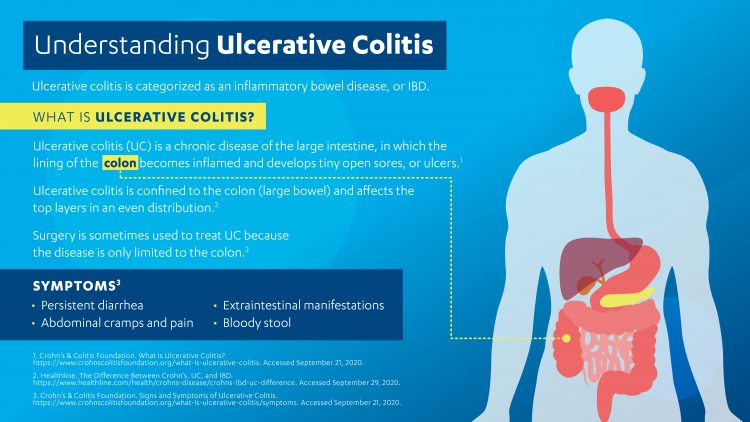
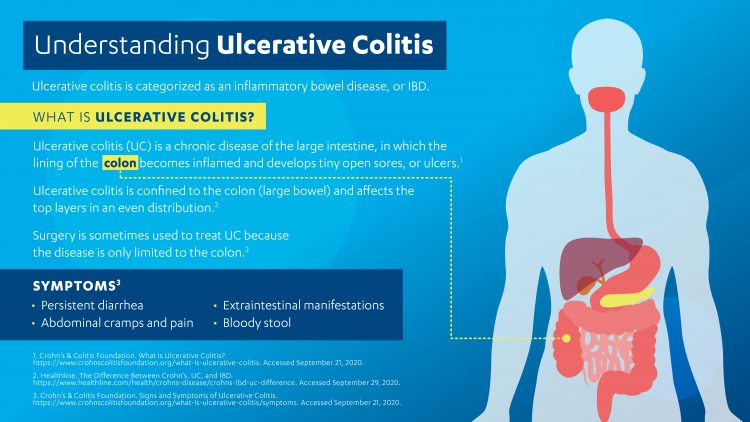
Currently, more than five million people around the world live with IBDs such as Crohn’s disease (CD) or ulcerative colitis (UC).1 The symptoms experienced by patients with UC are caused by inflammation and ulcers that occur along the mucosal lining of the large intestine and rectum and are driven by a dysregulated immune response.2 Disease onset can begin at any age, but most patients are young and experience symptoms before they reach the age of 30.3 Patients’ symptoms often have an unpredictable and recurrent course, which can have a devastating impact on their lives – including physical, psychological, sexual and social aspects.
Use of corticosteroids in the treatment armamentarium of UC
While not part of the primary medication regimen used to treat UC, corticosteroids are frequently prescribed to treat acute flares as they have broad anti-inflammatory activity and provide strong symptomatic relief to patients rapidly. However, they are not effective in preventing the progression of disease and their long-term use is associated with adverse side effects such as hyperglycaemia, weight gain, osteoporosis and other metabolic abnormalities, as well as sleep disturbances and changes in mood.6 In addition, corticosteroids leave individuals more susceptible to infection, including serious and opportunistic infections that can require more intensive and long term treatment.6 The risk and severity of these side effects is directly related to increased dose and duration of corticosteroid treatment.7
The long-term use of corticosteroids is not correlated with long-term remission in UC patients. Furthermore, misuse of corticosteroids is a significant limitation of current UC therapy as patients continue to receive prolonged treatment with corticosteroids. Within the first five years of diagnosis, one in eight individuals living with UC will demonstrate an inability to withdraw their use without the return of symptoms, resulting in corticosteroid dependence.6 One study found that 91 percent of dependency or excess use of corticosteroids prescribed in primary care was likely avoidable.6 Specific groups of patients, especially elderly people with IBD – the very group in whom chronic use of corticosteroids should be minimised or avoided – appear to be at an increased risk of misuse.6 Due to these risks, the decision to initiate treatment with corticosteroids should always be made carefully and alternate suitable options that avoid or minimise the use of corticosteroids should thus be considered where possible.
What does the future of UC treatment look like?
The future of UC treatment should focus on eliminating repeated or chronic dosing with corticosteroids by using effective and targeted medications, so that patients living with the disease are not compounding their burden with the substantial challenges of medication side effects and dependency. In chronic conditions like UC, where inflammation and symptoms occur when immune pathways become dysregulated, therapies are required that target the underlying pathways – not just those that offer quick symptomatic relief.
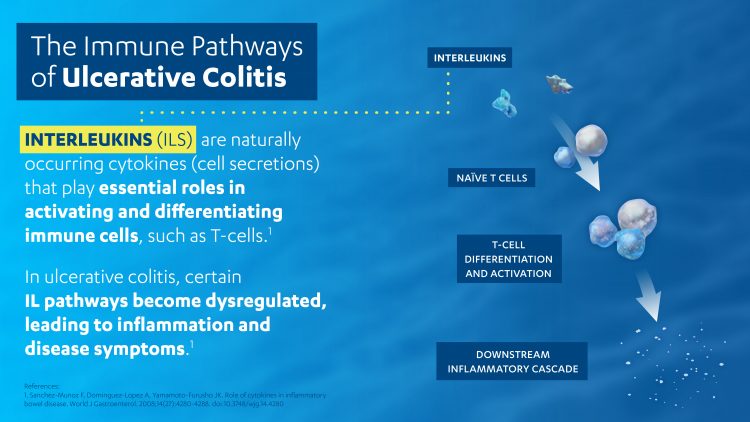
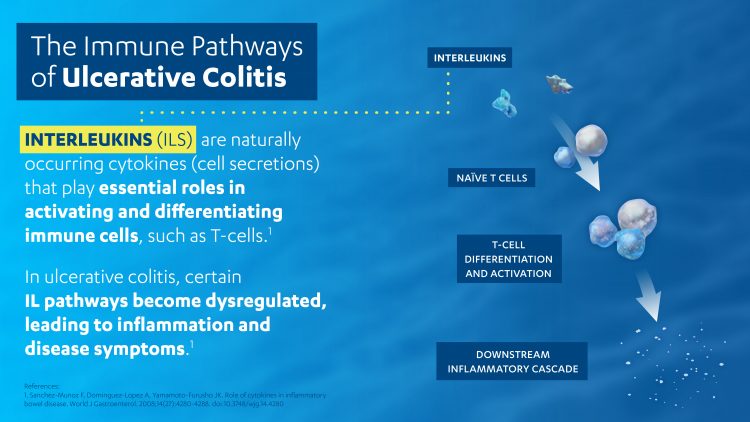
In recent decades, scientists have been uncovering the critical role that specific protein kinase pathways and interleukins (ILs) play in the pathophysiology of UC. As naturally occurring cytokines, research has revealed the important downstream impact of ILs on activating and differentiating specific immune cells such as T cells. Modulation of these pathways via therapeutics could therefore help the immune system to re-balance and regulate itself more effectively.8 Focusing on this immune system regulation and homeostasis can unlock a world of opportunity to advance research that focuses on better understanding patients’ immune systems, rather than on how to dull their symptoms.
Scientists are continuing to investigate the origins of IBDs, which are linked to damage of the intestinal epithelial barrier, to inform the development of more targeted therapies. At Janssen, we are also extending our research to explore how immune system balance can be restored in a damaged gut, either by enhancing or protecting a healthy epithelial barrier defence or by promoting a healthy microbiome.9 This vital research builds on our understanding of the pathogenesis of UC, enabling scientists to continue developing additional ways of re-establishing immune homeostasis for patients.
Novel pathway research will not only inform our understanding of IBDs and immune disorders more broadly, but also help us to provide additional options for patients who need them. The aim of treating IBD patients should be to enable them to live a highly productive life with minimal impact from disease or its treatment. It is a vital time for immunology research – the abundance of data, discoveries about the immune system’s function and actionable science are leading to amazing insights into the causes of disease, as well as to breakthroughs that could help more patients with immune-mediated diseases like UC to reach this goal.
About the author
Dr Chetan Karyekar is Compound Development Team Leader for the Janssen Pharmaceutical Companies of J&J, where he leads the largest brand in Janssen and J&J across all indications and functions. Chetan leads and oversees all R&D and life cycle management activities to bring a therapeutic asset from clinical development to patients and physicians. Prior to joining J&J, Chetan worked at Novartis and Bristol Myers Squibb. He earned his MD at the University of Mumbai and his PhD at the University of Maryland, Baltimore, before completing his residency at Chicago Medical School. His passion for developing new medicines is inspired by his experience helping patients as a clinical pharmacologist and seeing their unmet needs first-hand in clinic.
References
- The Facts About Inflammatory Bowel Diseases.Crohn’s & Colitis Foundation of America. Accessed June 2021. https://www.crohnscolitisfoundation.org/sites/default/files/2019-02/Updated%20IBD%20Factbook.pdf
- Ulcerative Colitis Treatment Options. Crohn’s & Colitis Foundation. Accessed June 2021. https://www.crohnscolitisfoundation.org/what-is-ulcerative-colitis/treatment-options
- Signs and Symptoms of Ulcerative Colitis. Crohn’s & Colitis Foundation. Accessed June 2021. https://www.crohnscolitisfoundation.org/what-is-ulcerative-colitis/symptoms
- What is Ulcerative Colitis? Crohn’s & Colitis Foundation. Accessed June 2021. https://www.crohnscolitisfoundation.org/what-is-ulcerative-colitis
- Hefti, M., et al. Severity of inflammation as a predictor of colectomy in patients with chronic ulcerative colitis. Dis Colon Rectum. 2009;52(2):193-197. doi:10.1007/DCR.0b013e31819ad456
- Blackwell, J., Selinger, C., Raine, T., et al. (2020). Steroid use and misuse: a key performance indicator in the management of IBD. Frontline Gastroenterology, 12(3), 207–213. https://doi.org/10.1136/flgastro-2019-101288
- Fact Sheet: Corticosteroids. Crohn’s & Colitis Foundation. Accessed June 2021. https://www.crohnscolitisfoundation.org/sites/default/files/legacy/corticosteroids.pdf
- Sanchez-Munoz F, Dominguez-Lopez A, Yamamoto-Furusho JK. Role of cytokines in inflammatory bowel disease. World J Gastroenterol. 2008;14(27):4280-4288. doi:10.3748/wjg.14.4280
- Brown, Jessica. Have IBD? Read About the Next Frontier in Disease Research That Taps Into the Microbiome. Johnson & Johnson, December 2, 2019. Accessed June 2021. https://www.jnj.com/innovation/next-frontier-ibd-research-gut-microbiome-treatments
Related topics
Disease research, Drug Development, Molecular Targets, Target Validation
Related conditions
Crohn’s disease (CD), Inflammatory bowel disease (IBD), ulcerative colitis (UC)


