An integrated vaccination approach to neurodegeneration
Posted: 23 September 2021 | Dr Andrea Pfeifer (AC Immune) | No comments yet
Guided by precise biomarker tests, therapeutic vaccines targeting the pathology of neurodegenerative disease could provide solutions to the impending global crisis in dementia. As Dr Andrea Pfeifer, Co-Founder, Chief Executive Officer and Director of AC Immune, describes here, current work is both establishing the targets that those vaccines must address and refining the techniques for addressing them.
The prevalence of dementia due to neurodegenerative conditions such as Alzheimer’s disease (AD) and Parkinson’s disease (PD) is expected to rise as life expectancy increases across the global population.1 Around 50 million people worldwide are already affected by dementia, a figure that is expected to nearly triple by 2050.2 Approximately 20 percent of women and 10 percent of men will develop AD,3 while PD affects over six million people making it the second most common neurodegenerative condition. Progressive memory loss, language processing impairment and dementia lead to a loss of independence and incur high costs in family-based or institutional care.
The prevalence of dementia due to neurodegenerative conditions such as Alzheimer’s disease (AD) and Parkinson’s disease (PD) is expected to rise as life expectancy increases across the global population.1 Around 50 million people worldwide are already affected by dementia, a figure that is expected to nearly triple by 2050.2 Approximately 20 percent of women and 10 percent of men will develop AD,3 while PD affects over six million people making it the second most common neurodegenerative condition. Progressive memory loss, language processing impairment and dementia lead to a loss of independence and incur high costs in family-based or institutional care.


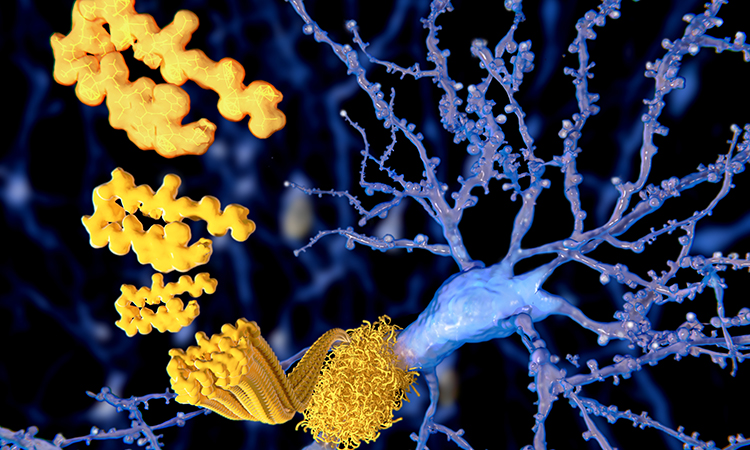
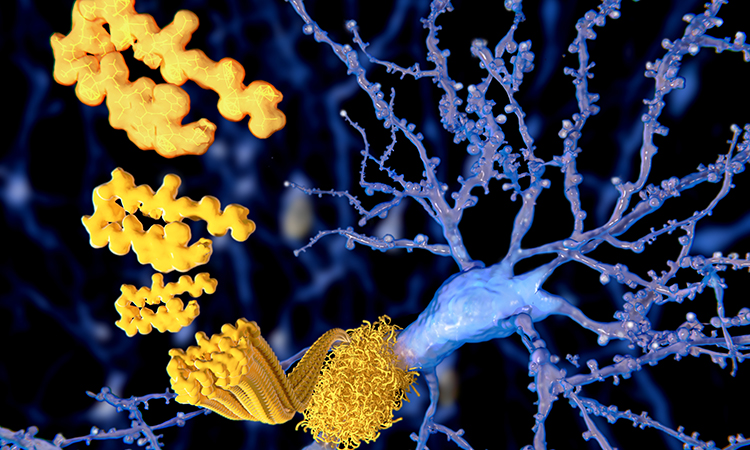
In AD, the most common protein aggregates are amyloid plaques formed of amyloid-beta (Aβ) and fibrous tangles of the protein tau that form within neurons and intracellular spaces.4 In PD, the aggregates are known as Lewy bodies and are formed principally of misfolded alpha-synuclein, which is also involved in the rarer condition, multiple system atrophy (MSA).
Vaccination and defining the correct neurodegeneration targets
In addressing neurodegenerative diseases, vaccines have several potential advantages as therapeutic entities over the passive antibody therapies that have so far garnered most public attention. Firstly, there are practical considerations such as the control and cost of manufacture and robust storage. Secondly, solutions such as vaccines that are deliverable through primary care settings rather than hospitals or infusion centres imply lower risk for frail or immunocompromised patients and will work both in developed and less-developed economies. There are potential advantages, too, in having the robust polyclonal response to a target antigen that a vaccine can provide.
In infectious diseases, the most appropriate target for vaccine development is usually readily definable. All COVID-19 vaccines, for instance, are centred around the Spike (S) protein of SARS-CoV-2, a prominent element of virus architecture that is functionally involved in infection. Once the virus sequence is elucidated, vaccine designs can begin almost immediately.
In neurodegenerative disease, however, the picture is more complicated. The hallmark protein aggregates are relatively well characterised but their contributions to the genesis and progression of individual patients’ disease are not well understood and may vary substantially from patient to patient.
There is strong in vivo evidence that Aβ, tau and alpha-synuclein (α-syn) promote each other’s aggregation through cross-seeding and other interactions, accelerating cognitive dysfunction5 and consequently complicating the disease process. In advanced disease, AD brains contain plaques but also other significant levels of other misfolded proteins, such as α-syn or TDP-43,6 thus addressing neurodegenerative diseases will likely require an armoury of therapies targeted at each of the principal underlying pathologies.
The need to understand which protein components contribute to individual patients’ disease is driving the development of blood-based assays that will enable the rational application of vaccines (or passive antibody therapies). These will enable clinicians to better match patients with therapies in clinical trials and subsequently the most appropriate treatments. They may also enable the much earlier detection of disease, perhaps pre-symptomatically when interventions may prove more effective.7
Defining protein targets at the conformational level
Another level of complexity must also be factored in; targets for degenerative disease vaccines are defined not only by the type of protein, but also by the precise conformation or derivative that is the toxic, disease-causative form of that protein.
At a minimal level, antibody and vaccine specificity must differentiate between the native form of a protein and misfolded forms of the same protein that share identical peptide sequences. Beyond that, however, protein misfolding is a progressive process involving many misfolded forms. Differentiating between those forms is also important in determining the effectiveness of any intervention. The pyroglutamate form of Aβ found in amyloid plaques as well as the oligomeric forms of Aβ, along with tau, are emerging as key targets in AD, as are certain phosphorylated types of tau.


All native proteins have essential roles in normal brain function. The amyloid precursor protein is a neuronal cell surface receptor, tau is an abundant axonal protein that helps assemble and stabilise microtubule and intracellular transport and α-syn is involved in the control of neurotransmitter release and synaptic plasticity.8 In general, while the native proteins are characterised by α-helices and random coils, the toxic insoluble forms are rich in β-structures9 with exposed hydrophobic regions that promote aggregation and seeding. However, there are intermediate forms, too – misfolded protein monomers transition to form oligomers and protofibrils. If not cleared by degradative mechanisms, these may progress into the less easily degraded forms – fibrils, aggregates or inclusions – that accumulate within and outside of neuronal cells, leading to dysfunction and neuronal cell death.10
Studies have shown that purified antibodies intended as therapeutics can be targeted specifically at chosen Aβ intermediates and that the range of targets can be broadened or narrowed by design. Solanezumab binds monomeric Aβ; bapineuzumab binds monomers, oligomers and fibrils; crenezumab preferentially binds to oligomeric over monomeric Aβ species; gantenerumab interacts preferentially with aggregated and oligomeric Aβ, while aducanumab binds oligomers and fibrils. Another therapeutic candidate, donanemab, was designed as a pyroglutamate Aβ antibody, a toxic form of Aβ enriched in plaques.
It is clear that target binding has a differential impact on protein aggregation. Solanezumab disrupts nucleation, gantenerumab and bapineuzumab block elongation of fibrils; aducanumab inhibits secondary nucleation,11 while crenezumab inhibits Aβ from forming toxic aggregates and oligomeric species and induces disaggregation of pre-formed aggregates.12
The clinical correlates of these distinctions remain incomplete, with the development of solanezumab and bapineuzeumab discontinued, aducanumab approved as a disease-modifying treatment for AD, donanemab about to embark on a large Phase III study and a crenezumab Phase II prevention study to complete next year. Amyloid clearance, cognitive consequences and the occurrence of a surrogate adverse event related to potential inflammation (ARIA-E) all appear to vary with the types of Aβ being targeted.
| Vaccine | Target | Status | Company |
| ACI 7104 | α-syn | PD Phase II | AC Immune |
| ABvac 40 | Amyloid | AD Phase II | Araclon Biotech |
| ACI-24 | Amyloid | AD Phase II; AD in Down’s Syndrome Phase Ib | AC Immune |
| UB-311 | Amyloid | AD Phase III | United Neuroscience |
| Lu AF20513 | Amyloid | AD Phase I | Lundbeck, Otsuka |
| AADvac1 | Tau | AD Phase II; Progressive Non-fluent Aphasia Phase I | Axon Neuroscience |
| ACI-35.030 | Tau | AD Phase I/II | AC Immune, Janssen |
Table 1: Neurodegenerative disease vaccine candidates in development
For the developers of therapeutic vaccines against neurodegenerative disease, the central message from the ongoing clinical studies in AD is that the ability to target the most toxic forms of misfolded protein selectively is vital for both efficacy and safety. The successes or travails of immuno-therapeutics may be instrumental in defining the precise targets that vaccine technologies must pursue.
Controlling conformation in vaccines for neurodegenerative diseases
In a modern approach, the antigenic elements of the vaccine must embody the structure and characteristics of the misfolded protein target. Furthermore, if the vaccine is to invoke the correct range of antibody and cellular responses, the misfolded protein structure presented by the vaccine must remain stable within the physiological environment of the human body.


One particularly innovative and proprietary technology platform retains and presents the misfolded β-sheet-rich conformations of neurodegenerative immunogens by anchoring antigens to the surface of a liposome. Using lipidated peptide residues at the ends of the peptide (or elsewhere), this strategy imposes a two-dimensional structure and stabilises the spatial arrangement of the antigen. Initial exploratory development compared two different liposomal constructs of Aβ. Both elicited fast immune responses in transgenic mouse models of AD but only the closely anchored conformation restored memory defects in mice.13 The approach was also effective in non-human primates14 and humans.15
The platform can be fine-tuned to elicit immune responses against specific conformation subtypes. By changing the pattern of peptides that are lipidated, the length of the lipid anchor or the surface charge on the liposome, the peptide conformation can be changed in a predictable manner. The degree of peptide aggregation can also be tuned using specific small molecules that interrupt the β-sheet arrangement.14
Several vaccine candidates utilising this technology are in clinical development. ACI-24, containing anchored Aβ,15 is in a Phase II trial in AD in the general population and in an earlier study of AD in Down’s syndrome. A liposomal vaccine containing a 16-mer tau peptide (ACI-35.030) is being tested in a Phase I/II study in early AD.16
An alternative technological approach for targeting the misfolded structure of native proteins is a form of molecular mimicry. This approach can be useful when targeting proteins with limited pathological variants such as α-syn, where immune tolerance may be difficult to break using native forms of a target protein. One method for breaking immune tolerance in this instance is to design vaccine epitopes that use novel peptide sequences. These can be selected using antibodies against the misfolded protein target as a template. The selected novel peptide fragments are neo-epitopes: they have the specific form of the protein driving the disease pathology but a distinct primary amino acid sequence.17 To create a vaccine, the peptide neo-epitope can be coupled to an immunogenic carrier, such as keyhole limpet haemocyanin, and formulated with a standard alum adjuvant. Selecting various carrier proteins while using this approach provides options to explore heterologous vaccination strategies that can optimise long-term maintenance of antibody responses to pathological protein species.
A vaccine made using the above approach demonstrated favourable safety and tolerability with no reported meningoencephalitis in a small Phase I AD trial but did not meet predefined outcome measures in the larger Phase II study. However, the platform continues to progress through the clinic for PD;18 the neo-epitope is an eight amino acid sequence that mimics the C-terminal region of human α-syn.
Additional vaccines that aim to address neurodegenerative diseases include two targeting tau that have reached Phase II studies in AD, as well as three, or possibly four, vaccines targeting Aβ that are in clinical development for the treatment of AD (see Table). There are also ongoing pre-clinical studies for vaccine programmes in Huntington’s disease.
Vaccination is a public health tool that can be deployed in tandem with advanced diagnostics for addressing the challenge of dementia through preventative precision medicine. The near-term vision is that genetics and population screening define the populations that can benefit while vaccination tailored for well-characterised neurodegenerative disease will preserve the health and independence of our ageing population.
About the author
Dr Andrea Pfeifer is the Chief Executive Officer and Director of AC Immune SA, having co-founded the company in 2003. Previously, she was the Head of Nestlé Research Centre, Switzerland, where she led the scientific development of several innovative products from laboratory to market, established the microbiome as a major cross-category product development platform and co-founded the Life Science-focused Nestlé Venture Capital Fund. She is currently a key member of the CEOi initiative on Alzheimer’s Disease and the Davos Alzheimer’s Collaborative (DAC). Andrea holds a PhD in toxicology (cancer research) from the University of Würzburg, Germany and is a registered Toxicologist and Pharmacist. She is also an Honorary Professor at the Ecole Polytechnique Fédérale de Lausanne (EPFL).
References
- GBD 2016 Dementia Collaborators. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(1):88-106. doi:10.1016/S1474-4422(18)30403-4
- Prince M, et al. World Alzheimer Report 2015. alzint.org/u/WorldAlzheimerReport2015.pdf
- Seshadri S, Wolf PA. Lifetime risk of stroke and dementia: current concepts, and estimates from the Framingham Study. Lancet Neurol. 2007;6(12):1106-1114. doi:10.1016/S1474-4422(07)70291-0
- Selkoe DJ. Folding proteins in fatal ways. Nature. 2003;426(6968):900-904. doi:10.1038/nature02264
- Clinton LK, et al. Synergistic Interactions between A-beta, tau, and alpha-synuclein: acceleration of neuropathology and cognitive decline. J Neurosci. 2010;30(21):7281-7289. doi:10.1523/JNEUROSCI.0490-10.2010
- Robinson JL, et al. Neurodegenerative disease concomitant proteinopathies are prevalent, age-related and APOE4-associated. Brain. 2018;141(7):2181-2193. doi:10.1093/brain/awy146
- Hansson O. Biomarkers for neurodegenerative diseases. Nat Med27, 954–963 (2021). https://doi.org/10.1038/s41591-021-01382-x
- Bogale TA, et al. Alpha-Synuclein in the Regulation of Brain Endothelial and Perivascular Cells: Gaps and Future Perspectives. Front Immunol. 2021;12:611761. Published 2021 Feb 19. doi:10.3389/fimmu.2021.611761
- Serpell LC, et al. Fiber diffraction of synthetic alpha-synuclein filaments shows amyloid-like cross-beta conformation. Proc Natl Acad Sci U S A. 2000;97(9):4897-4902. doi:10.1073/pnas.97.9.4897
- Yang HD, Ho DH, Yi MJ, et al. Misfolded Proteins in Neurodegenerative Dementias: Molecular Mechanisms. Dement Neurocogn Disord. 2012 Jun;11(2):38-52. https://doi.org/10.12779/dnd.2012.11.2.38
- Linse S, et al. Kinetic fingerprints differentiate the mechanisms of action of anti-Aβ antibodies. Nat Struct Mol Biol. 2020;27(12):1125-1133. doi:10.1038/s41594-020-0505-6
- Meilandt WJ, Maloney JA, Imperio J, et al. Characterization of the selective in vitro and in vivo binding properties of crenezumab to oligomeric Aβ. Alzheimers Res Ther. 2019;11(1):97. Published 2019 Dec 1. doi:10.1186/s13195-019-0553-5
- Muhs A, et al. Liposomal vaccines with conformation-specific amyloid peptide antigens define immune response and efficacy in APP transgenic mice. Proc Natl Acad Sci U S A. 2007;104(23):9810-9815. doi:10.1073/pnas.0703137104
- Hickman DT, et al. Sequence-independent control of peptide conformation in liposomal vaccines for targeting protein misfolding diseases. J Biol Chem. 2011;286(16):13966-13976. doi:10.1074/jbc.M110.186338
- National Library of Medicine (U.S.) (2019, July) A Study to Evaluate the Safety, Tolerability and Immunogenicity of Tau Targeted Vaccines in Participants With Early Alzheimer’s Disease. Identifier NCT04445831. https://clinicaltrials.gov/ct2/show/NCT04445831
- Theunis C, et al. Efficacy and safety of a liposome-based vaccine against protein Tau, assessed in tau.P301L mice that model tauopathy. PLoS One. 2013;8(8):e72301. Published 2013 Aug 19. doi:10.1371/journal.pone.0072301
- Schneeberger A, et al. AFFITOME® technology in neurodegenerative diseases: the doubling advantage. Hum Vaccin. 2010;6(11):948-952. doi:10.4161/hv.6.11.13217
- Volc D, et al. Safety and immunogenicity of the α-synuclein active immunotherapeutic PD01A in patients with Parkinson’s disease: a randomised, single-blinded, Phase I trial. Lancet Neurol. 2020;19(7):591-600. doi:10.1016/S1474-4422(20)30136-8
Related topics
Drug Targets, In Vivo, Neurons, Neuroprotection, Neurosciences, Protein, Target molecule, Vaccine
Related conditions
Alzheimer's disease (AD), Dementia, Huntington's disease
Related organisations
AC Immune SA, IDBS


