Targeting phosphodiesterase 3A: discovery of a promising cancer therapy
Posted: 22 June 2021 | Dr Harri Sihto (University of Helsinki), Dr Katja Ivanitskiy (Sartar Therapeutics), Professor Olli Kallioniemi (Sartar Therapeutics) | No comments yet
A new promising sarcoma target, phosphodiesterase 3A (PDE3A), and drugs targeting it have been identified by researchers at the University of Helsinki. Dr Katja Ivanitskiy, Dr Harri Sihto and Professor Olli Kallioniemi outline emerging evidence that indicates PDE3A protein-targeting compounds may induce sarcoma cell death by acting as a molecular glue between PDE3A and Schlafen 12 proteins.
Local soft-tissue sarcomas can be treated with surgery and adjuvant radiotherapy. However, almost half of sarcomas advance locally or develop metastases, resulting in significantly reduced five-year survival rates.3 The five‑year survival rates for local, regional and metastatic soft-tissue sarcomas are approximately 81 percent, 56 percent and 15 percent, respectively.4 Most advanced soft-tissue sarcomas are treated by surgery and doxorubicin‑based therapy, developed in the 1970s and still considered as a standard therapy for these tumours. Despite the somewhat increased selection of available treatment options available, the current chemotherapy regimens have not truly improved the overall survival of patients. They are mainly used as a palliative therapy for metastatic soft-tissue sarcomas and in advanced disease, where a median survival of only 12-18 months is achieved with treatment.3,5
Our promising results in pre-clinical studies are now leading the way towards clinical trials”
Only a few breakthroughs have been made in the area of personalised sarcoma medicine. In gastrointestinal stromal tumours (GIST), the discovery of mutated KIT and PDGFRA genes led to the introduction of tyrosine kinase inhibitor therapies, such as imatinib, which have dramatically improved patient outcomes during the past two decades. Unfortunately, GISTs frequently become resistant to all kinase inhibitors and therefore novel therapy targets and new treatment options are urgently required for GIST and other soft-tissue sarcomas.
PDE3A as a target for cancer therapy
PDE3A is an enzyme that catalyses hydrolysis of cyclic adenosine monophosphate (AMP) and cyclic guanosine monophosphate (GMP) – the two important second messengers in cells. It regulates biological functions such as vasodilation, vascular smooth muscle contraction and platelet formation. Several recent studies have suggested that PDE3A is also a potential drug target in cancer and that different compounds targeting PDE3A are able to reduce cancer cell survival.
Our study discovered that PDE3A is exceptionally highly expressed in GIST as compared to all other tumour types or healthy tissues, making the enzyme a promising emerging target for sarcoma therapy.
Discovery of a promising compound
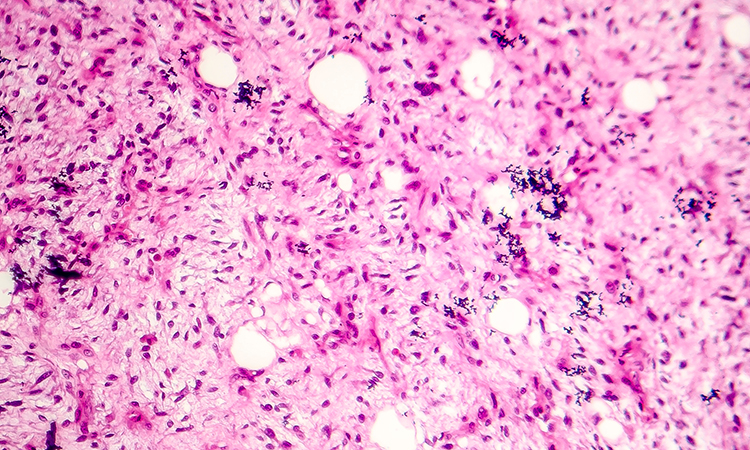
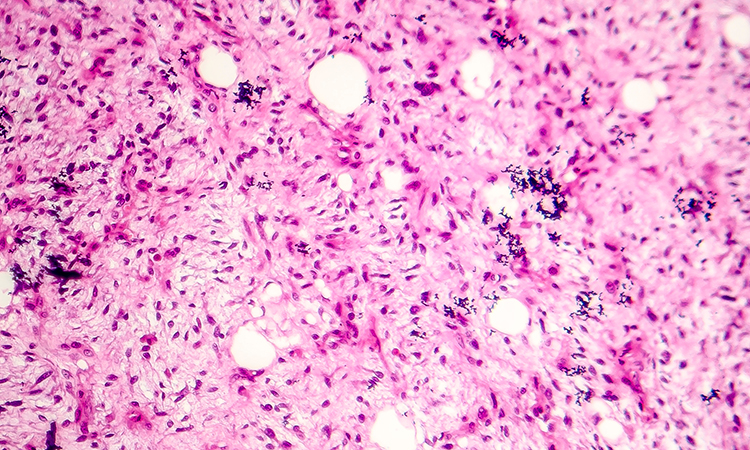
From these findings, we went on to discover that the PDE3A-targeting compound anagrelide hydrochloride, a drug that has been used to reduce platelet levels in essential thrombocythaemia, effectively killed GIST cancer cell lines and patient-derived tumour xenografts in vivo.6 The discovery was made by molecular and functional data integration across a large number of targets, drugs and indications, using research tools developed at the Institute of Molecular Medicine Finland. A database of the human transcriptome was utilised to discover GIST-specific gene overexpression among 20,000 tissue samples from 200 healthy and cancerous tissue types. In parallel, 230 compounds were screened for efficacy in GIST cell lines. The analysis pipeline was further enhanced by RNA-sequencing and immunohistochemistry-based data obtained from archived formalin-fixed tissue samples.


In addition to GIST, other soft-tissue sarcoma types may also be potential targets for PDE3A-targeted therapies. Overall, these studies indicate the power of large-scale molecular and functional (drug response) data in identifying druggable opportunities as well as compounds and drugs that could be further developed. The large number of various tissue types included in the computational analyses also make it possible to predict possible off-target effects of the drugs and archived biobank materials enable study of large series of rare cancers.
Besides the generic anagrelide, an approved drug, many other compounds such as 6-(4-(diethylamino)-3-nitrophenyl)-5-methyl-4,5-dihydropyridazin-3(2H)-one (DNMDP), 17-β-estradiol and its related steroid hormones, as well as nauclefine, from a Nauclea latiafolia plant extracted alkaloid, have shown to induce cell death through PDE3A.7-9 A common feature among all these compounds is that they act as a molecular glue by inducing complex formation of PDE3A and Schlafen 12 (SLFN12) proteins.7-10 Cell apoptosis is driven independently from PDE3A enzyme activity and, indeed, other PDE3-specific enzyme inhibitors such as cilostazol or milrinone are not able to cause cell death in PDE3A‑positive cancer cell lines.4,5 PDE3A‑SLFN12 complex formation therefore leads to translational downregulation of anti‑apoptotic Bcl-2 and Mcl-1 proteins in the endoplasmic reticulum.9 These newly found mechanisms provide opportunities to target GIST and other PDE3A overexpressing cancers via emerging and established drugs.
What is next?
PDE3A is exceptionally highly expressed in GIST as compared to all other tumour types or healthy tissues”
As an already approved drug, the pharmacokinetics and safety profile of anagrelide is well known in humans, which therefore provides opportunities for fast repurposing of the drug for PDE3A‑positive cancers such as GIST. A spin-out company, Sartar Therapeutics Ltd, was founded by the researchers of University of Helsinki, developing the first candidate product SAR001 – a subcutaneously administrated controlled-release formulation for the treatment of GIST. The new formulation improves the pharmacokinetic properties of anagrelide and mitigates the high plasma concentration peaks and fast turnover seen in oral dosing. Our promising results in pre-clinical studies are now leading the way towards clinical trials. With an effective and validated research pipeline in place, we are also seeking to explore further opportunities for new cancer treatments in future.
About the authors






References
- WHO Classification of Tumours Editorial Board. WHO Classification of Tumours of Soft Tissue and Bone, 5th ed. Lyon, France: IARC Press; 2020.
- Stiller CA, Trama A, Serraino D, et al. Descriptive epidemiology of sarcomas in Europe: Report from the RARECARE project. Eur J Cancer 2013, 49; 684-95.
- Italiano A, Mathoulin-Pelissier S, Le Cesne A, et al. Trends in survival for patients with metastatic soft‑tissue sarcoma. Cancer 2011, 117; 1049-54.
- The National Cancer Institute (NCI), Surveillance, Epidemiology and End Results Database: https://www.cancer.org/cancer/%20soft-tissue-sarcoma/detection-diagnosis-staging/survival-rates.html
- Karavasilis V, Seddon BM, Ashley S, et al. Significant clinical benefit of first-line palliative chemotherapy in advanced soft-tissue sarcoma: retrospective analysis and identification of prognostic factors in 488 patients. Cancer 2008, 112; 1585-1591.
- Pulkka OP, Gebreyohannes YK, Wozniak A, et al. Anagrelide for gastrointestinal stromal tumor. Clin Cancer Res 2019, 25; 1676-1687.
- de Waal L, Lewis TA, Rees MG, et al. Identification of cancer cytotoxic modulators of PDE3A by predictive chemogenomics. Nat Chem Biol 2016, 12; 102-108.
- Ai Y, He H, Chen P, et al. An alkaloid initiates phosphodiesterase 3A-Schlafen 12 dependent apoptosis without affecting the phosphodiesterase activity. Nature Commun 2020, 11; 3236.
- Li D, Chen J, Ai Y, et al. Estrogen-Related Hormones Induce Apoptosis by Stabilizing Schlafen-12 Protein Turnover. Mol Cell 2019, 75; 1103-1116e9.
- Chen J, Liu N, Li D, et al. Complex structure of PDE3A-SLFN12 and structure-based molecular glue design, for apoptosis of tumor cells. Nature Portfolio, reprint
Related topics
Drug Development, Drug Discovery, Oncology, Screening, Small Molecules
Related conditions
Cancer, Gastrointestinal stromal tumours (GIST), sarcoma
Related organisations
Beckman Coulter, Horizon Discovery, Institute of Molecular Medicine Finland, Merck, X-Chem


