Could dolphins be viable models for human brain disorders?
Posted: 25 February 2020 | Professor Giovanni Di Guardo (University of Teramo) | No comments yet
Neuropathologic similarities between dolphins and humans suggest that the former could act as an effective model for the study of diseases such as Alzheimer’s. Professor Giovanni Di Guardo explains why dolphins could provide researchers with a new window into neurodegenerative conditons.


A number of spontaneously occurring diseases in dolphins, of both infectious and non-infectious nature, share pathologic similarities with human conditions.
For example, the highly pathogenic agent Cetacean morbillivirus (CeMV) has caused several cetacean mass mortality outbreaks across the globe over the last 30 years. The impacts of this virus have been particularly severe among bottlenose dolphins (Tursiops truncatus) along the Eastern US coastline, as well as among striped dolphins (Stenella coeruleoalba) and long-finned pilot whales (Globicephala melas) in the Western Mediterranean Sea.1
Similarly to events observed in human patients infected by its closely related ‘cousin’, the Measles virus (MeV), CeMV-infected dolphins exhibit pathologic changes consistent with the lymphotropic, epitheliotropic and neurotropic ‘attitudes’ commonly displayed by these two pathogens and more generally by Morbillivirus genus members. These include a prominent immune cell destruction and loss within secondary lymphoid tissues, accompanied by a bilateral broncho/bronchiolo-interstitial pneumonia, as well as a non-suppurative (meningo)-encephalitis. Infected cells additionally show intracytoplasmic and/or endonuclear viral inclusion bodies, while giving rise to multinucleated syncytia-harbouring levels of CeMV antigen.2
Taking CeMV neurotropism into special consideration, it is worth mentioning that a viral strain termed Dolphin morbillivirus (DMV), which has been responsible for at least four “unusual mortality events” among Western Mediterranean striped dolphins throughout the last three decades, has also caused a peculiar, brain-only form of DMV infection (BOFDI). Noteworthily, BOFDI-affected dolphin specimens develop brain lesions that are morphologically consistent with those found in MeV-infected, subacute sclerosing panencephalitis (SSPE)-affected humans.


Another relevant issue, still belonging to the challenging topic of comparative neuropathology, concerns Alzheimer’s disease, the most frequent type of human dementia worldwide.4 For a very long time, the global research community has been extensively seeking appropriate experimental and natural animal models that reliably encompass the peculiar Alzheimer’s lesion spectrum, namely amyloid-ß extra-neuronal plaques and tau protein neurofibrillary tangles.4
Recently, for the first time in any wild animal species, amyloid-ß and tau deposits have been simultaneously reported within the brain tissues of bottlenose dolphins and striped dolphins stranded along the Spanish coastline.5 Additionally of interest for researchers are the cerebral amyloid-ß plaques and associated neuropathological changes described in bottlenose dolphins beached along the US Atlantic coast, which also harboured consistent levels of β-methylamino-L-alanine (βMAA), a cyanobacterial neurotoxin.6
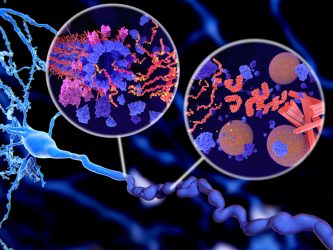
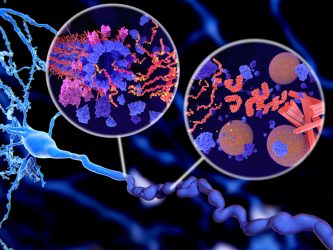
Although its biological functions have thus far only been uncovered to a limited extent, PrPC has been reported to act as a pivotal neuron cell receptor for amyloid-ß, with PrPC– amyloid-ß interaction(s) also responsible for the synaptic dysfunction(s) commonly detected in Alzheimer’s-affected patients.8 Therefore, if similar PrPC– amyloid-ß relationships were documented in the brain tissue from the aforementioned stranded cetacean specimens,5,6 this would contribute to qualify bottlenose dolphins and striped dolphins as valuable and reliable natural disease models for the comparative neuropathological and neuropathogenetic study of Alzheimer’s in humans.
The two dolphin and human neuropathy examples described above should be regarded as a ‘window’ on several disease conditions, of either neurologic or non-neurologic origin, for which cetaceans may serve as potential comparative pathology models when investigating their human disease analogues.
Therefore, stranded cetaceans may play a crucial role as potentially useful comparative neuropathology models for the study of their human neurological disease counterparts.
About the author
Professor Giovanni Di Guardo graduated in Veterinary Medicine in 1982 at the University of Bologna, Italy. In 1995, he was appointed Diplomate of the European College of Veterinary Pathologists. Since February 2002, he has served as an Associate Professor at the Veterinary Medical Faculty of the University of Teramo, Italy, where he teaches on the main course of General Pathology and Veterinary Pathophysiology. Di Guardo has authored/co-authored over 500 scientific works, 150 of which are published in international, peer-reviewed journals.
References
- Di Guardo G. Cetaceans, models for human disease? Res Vet Sci 2018;119:43-44.
- Di Guardo G, Marruchella G, Agrimi U, Kennedy S. Morbillivirus infections in aquatic mammals: A brief overview. J Vet Med Physiol Pathol Clin Med 2005;52:88-93.
- Lucá R, Giacominelli-Stuffler R, Mazzariol S, Roperto S, Cocumelli C, Di Guardo G. Neuronal and astrocytic involvement in striped dolphins (Stenella coeruleoalba) with morbilliviral encephalitis. Acta Virol 2017;61:495-497.
- Querfurth HW, LaFerla FM. Alzheimer’s disease. N Engl J Med 2010;362:329-344.
- Gunn-Moore D, Kaidanovich-Beilin O, Gallego Iradi MC, Gunn-Moore F, Lovestone S. Azheimer’s disease in humans and other animals: A consequence of postreproductive life span and longevity rather than aging.Alzheimers Dement 2018;14:195-204.
- Davis DA, Mondo K, Stern E, et al. Cyanobacterial neurotoxin BMAA and brain pathology in stranded dolphins. PLoS One 2019;14(3):e0213346.
- Di Guardo G. Alzheimer’s disease, cellular prion protein, and dolphins. Alzheimers Dement 2018;14:259-260.
- Lauren J, Gimbel DA, Nygaard HB, Gilbert JW, Strittmatter SM. Cellular prion protein mediates impairment of synaptic plasticity by amyloid-β oligomers. Nature 2009;457:1128-1132.
Related topics
Disease research, Neurons, Neurosciences, Research & Development, Therapeutics
Related conditions
Alzheimer’s disease, subacute sclerosing panencephalitis (SSPE)


