Novel anti-inflammatory slows progression of MS in mice
Posted: 22 October 2020 | Hannah Balfour (Drug Target Review) | No comments yet
When delivered intranasally, the anti-inflammatory drug VX-765 prevented axon demyelination and loss in a murine model of multiple sclerosis (MS).
In a murine model of multiple sclerosis (MS), intranasal administration of an experimental anti-inflammatory drug called VX-765 helped prevent damage to neurons, effectively slowing the progression of the disease.
MS is a neurodegenerative disease with no known cause or cure. Christopher Power, a professor in the Faculty of Medicine & Dentistry at the University of Alberta (U of A), US, and his lab seek to better understand the disease and use this knowledge to develop effective treatments.
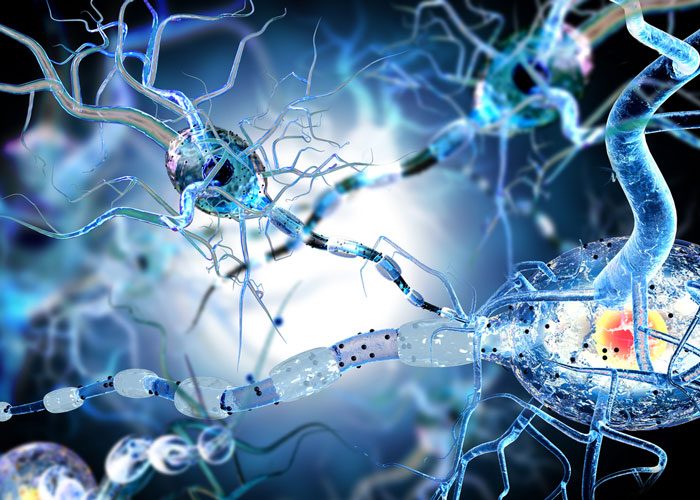
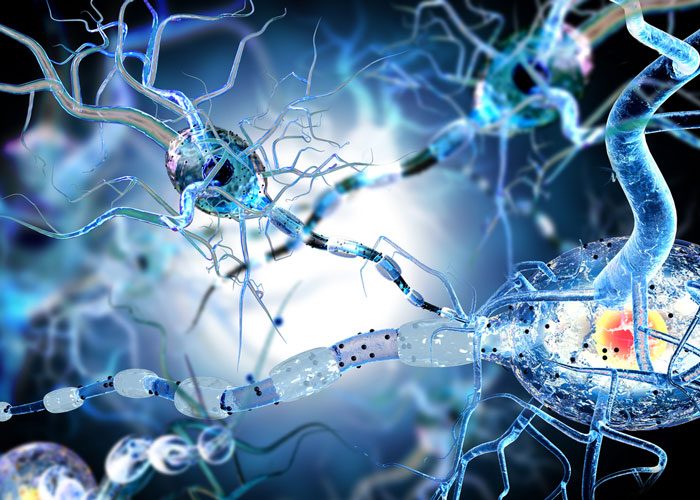
“Nerves in the brain are like insulated wires, but in MS there is initially a loss of the insulation [called myelin], and then the eventual loss of the wire. Those losses are caused by inflammation. That inflammation, which we think is the driving force for MS, is our main research interest,” said Power, who is also a neurologist in the Northern Alberta MS Clinic, co-director of the U of A’s MS Centre and a member of the Neuroscience and Mental Health Institute.
His research group is particularly interested in inflammasomes, molecules that are responsible for the activation of an inflammatory response in the body. Because it is believed that chronic inflammation plays a role in the progression of MS, targeting the inflammasome – and by connection controlling the inflammatory response – may be able to halt disease progression. Power’s lab identified VX-765 as a strong candidate therapy for MS patients.
The drug works by inhibiting caspase-1, a component of inflammasomes that promotes harmful inflammation in the body. They decided to administer VX-765 intranasally because of previous success when delivering insulin in the same manner to control brain inflammation. To do this they first had to dissolve VX-765 in a fluid and then injected the mixture into the nose of mice.
Commenting on the intranasal delivery method, Power said: “It is a lot easier for patients because you need less of the drug. It is a direct delivery into the brain, it does not go into the circulatory system and it is not broken down as quickly.”
By collaborating with researcher Frank Wuest, interim chair in the U of A’s Department of Oncology and member of the Cancer Research Institute of Northern Alberta, Power’s lab were able to examine the impact of VX-765 on nerves. Wuest is a world expert on positron emission tomography (PET) scanning, an imaging technique that uses radioactive substances to visualise changes in the body. Using PET scans to image brain metablolism, Wuest was able to document whether the myelin sheath surrounding the neurons had been stripped or not after the therapeutic was delivered.
Power concluded: “The study shows intranasal therapy is effective in preventing demyelination, axon injury and loss… The loss of myelin and loss of nerves are irreversible processes, so any therapeutic that helps to slow or prevent that from happening is an exciting advance for MS research. The particular delivery method also allows the therapy to be delivered in a more precise and targeted way.”
The study was published in GLIA.
Related topics
Disease research, Drug Development, Drug Leads, In Vivo, Neuroprotective compounds, Neurosciences, Research & Development, Therapeutics
Related conditions
Multiple Sclerosis (MS)
Related organisations
University of Alberta
Related people
Christopher Power, Frank Wuest



