Bionic liver organs explain toxicity of paracetamol
Posted: 17 August 2015 | Victoria White
Scientists have created a liver-on-chip device mimicking human physiology, leading to the discovery of a new mechanism of paracetamol toxicity…
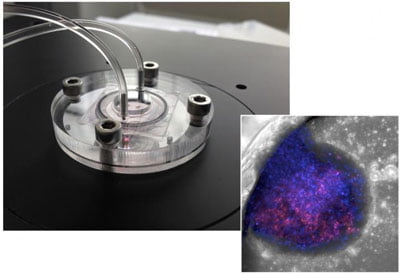
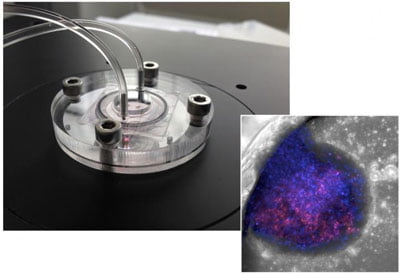
Liver-on-chip device and microscopic image of bionic liver. CREDIT: Yaakov Nahmias / Hebrew University
In recent years there is a growing understanding that animal experiments may fail to predict the human response, necessitating the development of alternative models to predict drug toxicity.
The main challenge in replacing animal experiments is that human cells seldom survive more than a few days outside the body. To address this challenge, scientists at the Hebrew University of Jerusalem and the Fraunhofer Institute for Cell Therapy and Immunology partnered to create a liver-on-chip device mimicking human physiology.
“The liver organs we created were less than a millimetre in diameter and survive for more than a month,” said Professor Yaakov Nahmias, Director of the Alexander Grass Centre for Bioengineering at the Hebrew University.
The breakthrough came when the group added nanotechnology-based sensors to the mix. “We realised that because we are building the organs ourselves, we are not limited to biology, and could introduce electronic and optical sensors to the tissue itself. Essentially we are building bionic organs on a chip,” said Nahmias.
The addition of nanotechnology-based optoelectronic sensors to the living tissues enabled the group to identify a new mechanism of paracetamol (acetaminophen) toxicity.
“Because we placed sensors inside the tissue, we could detect small and fast changes in cellular respiration that nobody else could,” said Nahmias.
Global market for human-on-a-chip technology estimated to grow to $17b by 2018
The researchers discovered that acetaminophen blocked respiration, much faster and at a much lower dose than previously believed. The current understanding was that acetaminophen was broken to a toxic compound, called NAPQI, before damaging the cells. As the liver could naturally deactivate NAPQI, damage was thought to occur only at high doses and in cases of diseased or compromised liver function.
The current study turns 50 years of research on its head. The authors found that acetaminophen itself can stop cellular respiration in minutes, even in the absence of NAPQI, explaining much of the off target effects of the drug.
“This is a fascinating study,” said Professor Oren Shibolet, Head of the Liver Unit at the Tel-Aviv Sourasky Medical Centre, and one of the leading experts on drug-induced liver injury, who was not involved in the original study. “We knew that acetaminophen can cause nephrotoxicity as well as rare but serious skin reactions, but up until now, we didn’t really understand the mechanism of such an effect. This new technology provides exceptional insight into drug toxicity, and could in fact transform current practice.”
The results mark the first discovery of a new toxicity mechanism using the newly emerging human-on-a-chip technology, suggesting that the development of alternative models for animal testing is just around the corner. The global market of this technology is estimated to grow to $17 billion by 2018, showing a double-digit annual growth rate in the last three years.
The study findings are published in Archives of Toxicology.
Related topics
Organ-on-a-Chip
Related conditions
HIV
Related organisations
Hebrew University of Jerusalem


