Researchers uncover the signals that govern the fate of TFH cells
Posted: 31 July 2015 | Victoria White
Researchers identify a pair of master regulators that control the fate of follicular helper T (TFH) cells – a finding that could improve vaccine design…
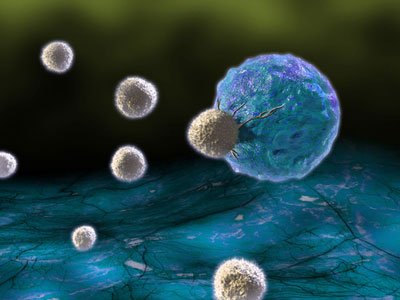
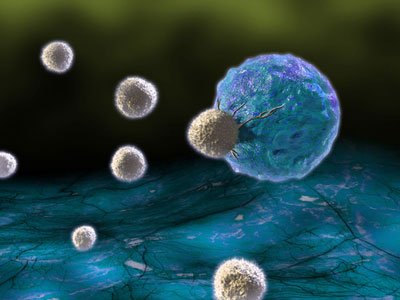
A team of researchers at the La Jolla Institute for Allergy and Immunology has identified a pair of master regulators that control the fate of follicular helper T (TFH) cells.
TFH cells are a rare type of immune cell that is essential for inducing a strong and lasting antibody response to viruses and other microbes.
The researchers’ finding holds great promise for improved vaccine design and may lead to new treatments for immune disorders and possibly even cancer.
“Almost all licensed human vaccines work on the basis of inducing a long-term, protective antibody response,” explained Shane Crotty, Ph.D., a professor in the Institute’s Division of Vaccine Discovery. “Being able to enhance or increase the frequency of follicular helper T cells may be an excellent approach for better vaccine design.”
Before B cells can launch a full-blown antibody response against invading pathogens they undergo a tightly orchestrated, multi-step maturation process aided by TFH cells. This process selectively promotes the proliferation of B cells that produce high-affinity antibodies and weeds out those that produce less potent ones.
“B cells compete for TFH cells to survive,” explained postdoctoral researcher Youn Soo Choi, Ph.D., “Only those B cells that produce highly specific antibodies attract TFH cells and are able to proliferate.” The survivors undergo successive rounds of mutation and selection resulting in better and better antibodies during the course of an immune response.
Defects in TFH function or frequency can have dramatic effects
“TFH cells are essential for the production of most types of antibodies and defects in TFH function or frequency can have dramatic effects,” says Crotty. “It may be particularly important when antibody targets are difficult to recognize and B cells need to explore a bigger mutational landscape. A better understanding of how these cells are produced could really make a difference in how likely it is that your body manages to make good antibodies against an infection.”
In an earlier study, Crotty’s team had identified the BCL6 gene as a crucial mastermind in the differentiation of TFH cells but important pieces of the puzzles had still been missing. A combination of functional genomics and bioinformatics analysis allowed Choi to narrow the list of potential candidates down to a pair of transcription factors, LEF-1 and TCF-1. Transcription factors act as master switching by binding to regulatory regions in the genome, where they modulate gene activity. He then confirmed the importance of LEF-1 and TCF-1 for the differentiation of TFH cells with the help of mice genetically engineered to lack the genes encoding either LEF-1 or TCF-1.
“Their activity pre-programs CD4+ T cells to respond to TFH induction signals,” said Choi. “It seems very likely that any perturbation that results in lower levels of these transcription factors could decrease the likelihood that T cells differentiate into TFH cells.”
As a matter of fact, individual differences in the predilection to make more TFH cells could explain why some individuals produce highly efficient antibodies against HIV, while most individuals are unable to mount a potent immune response. “It is very difficult to create high-affinity antibodies for HIV, which are necessary to neutralise virus,” explained Crotty. “Interestingly, it turns out that those individuals that are able to make broadly neutralising antibodies against HIV, have unusually elevated levels of highly functional memory TFH cells. We speculate that these people may have a genetic bias to produce a really good TFH response but we haven’t identified it yet.”
The research findings are published in Nature Immunology.
Related topics
Antibody Discovery, Genomics, Immunology
Related conditions
HIV
Related organisations
Cancer Research, La Jolla Institute for Allergy and Immunology


