Skeletal stem cells de-differentiate to achieve extensive growth
Posted: 1 November 2018 | Drug Target Review | No comments yet
Researchers in the U.S. have discovered that skeletal stem cells in the jaws of adult mice de-differentiate when tasked with regenerating large portions of bone and tissue.
The finding is the first to show that mammalian skeletal stem cells can march backward along the developmental timeline and de-differentiate – a process in which they become more primitive in response to environmental signals. Specifically, the cells appeared to regress to a cell type that normally occurs within weeks of conception in humans and that gives rise to the bones, cartilage and connective tissue in the head and face.
The results – obtained by researchers at the Stanford University School of Medicine – suggest the possibility of using naturally occurring adult stem cells, which are usually restricted to generating only a limited panel of closely related progeny, to carry out more extensive regeneration projects throughout the body.
Commenting on the impact of their discovery, Michael Longaker MD, professor of plastic and reconstructive surgery, said: “It’s pretty remarkable that this would happen in an adult animal,”
“It changes the way we look at skeletal development and regeneration.”
Longaker, the Deane P. and Louise Mitchell Professor in the School of Medicine and co-director of the Stanford Institute for Stem Cell Biology and Regenerative Medicine, shares senior authorship with Howard Chang MD PhD, professor of dermatology and of genetics and director of Stanford’s Center for Personal Dynamic Regulomes. Graduate students Ava Carter and Ryan Ransom are the lead authors.
The researchers were studying a common surgical technique called distraction osteogenesis, which is often used in newborns or infants to lengthen abnormally-stunted bones in the lower jaw. These malformations occur in conditions such as Pierre-Robin sequence, Treacher Collins syndrome and craniofacial microsomia.
During distraction osteogenesis, the bone is surgically fractured, and an adjustable device is inserted to gradually increase the distance between the ends of the bone over the course of weeks. This encourages new bone growth to fill in the gap and create what resembles a normally developed mandible.
“This is a very special system of regeneration that echoes what normally happens in development,” said Chang, who is the Virginia and D.K. Ludwig Professor of Cancer Genomics and a Howard Hughes Medical Institute investigator. “If you cut the bone, and stretch it, you get more bone. But this regeneration requires mechanical force. We wanted to know how skeletal stem cells respond to this kind of environmental signal.”
Recently, Stanford researchers identified the skeletal stem cell in both mice and humans. Like other stem cells that occur in adult animals, skeletal stem cells are restricted in their ability to generate different cell types. In particular, they can generate bone, cartilage and stroma (the bone’s spongy interior) to repair normal damage like fractures. However, the regeneration required by distraction osteogenesis, in which the bone ends are repeatedly moved further apart, is far more extensive.
“How do they know to reform a mandible with the correct shape and function?” questioned Longaker. “Are they simply recapitulating normal development? And, if so, how?”
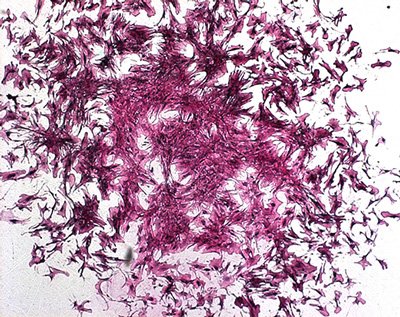
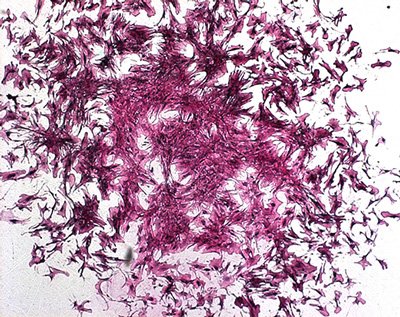
Carterand Ransomused a technique developed in the Chang laboratory called ATAC-seq to identify gene switches that are turned on in mouse skeletal stem cells in response to the mechanical force of distraction. They found that the cells began to express genes normally found in cranial neural crest cells – cells that arise in humans about five to six weeks after conception and that form the bones, cartilage and connective tissue of the head and face. At the same time, the cells tamped down the expression of genes involved in normal fracture repair.
“This was really a surprise,” Longaker said. “These cells appear to revert back to a cell type responsible for forming the jaw during early development. That’s why the regenerated mandible looks like one formed in early embryogenesis.”
In the absence of mechanical force to separate the bone, the skeletal stem cells repaired the fracture without expressing cranial neural crest genes.
Further research identified the focal adhesion kinase molecular pathway as a key player in the ability of the skeletal stem cells to detect and respond to mechanical force. Inhibiting this pathway removed the cells’ ability to make new bone during distraction osteogenesis.
The researchers believe the finding has provocative clinical implications.
“Now that we’ve identified one of the molecular pathways responsible for this developmental shift, it may be possible to target the proteins in that pathway to achieve a similar outcome without the requirement for physical force,” Carter said.
“We’re beginning to understand in detail how skeletal stem cells are likely to respond to environmental cues in humans,” Longaker said. “This is an opportunity to change how we think about the development of not just the skeleton, but also other tissues and organs. Can we go back in time after an organ is formed to trigger more extensive regeneration? This at least opens the door to that possibility.”
Details of this research were published in Nature.
Related topics
Regenerative Medicine, Research & Development, Sequencing, Stem Cells
Related conditions
craniofacial microsomia, Pierre-Robin sequence, Treacher Collins syndrome
Related organisations
Stanford University School of Medicine
Related people
Ava Carter, Howard Chang MD PhD, Michael Longaker MD, Ryan Ransom



