Therapy stops treatment-resistant glioblastoma and high-grade gliomas
Posted: 9 May 2016 | Victoria White, Digital Content Producer | No comments yet
In laboratory tests on human cells and mouse models, an experimental therapy was shown to stop treatment-resistant glioblastoma and high-grade gliomas…
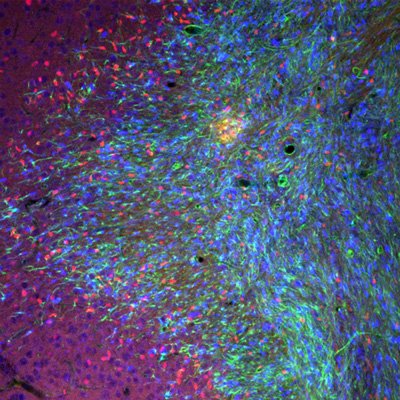
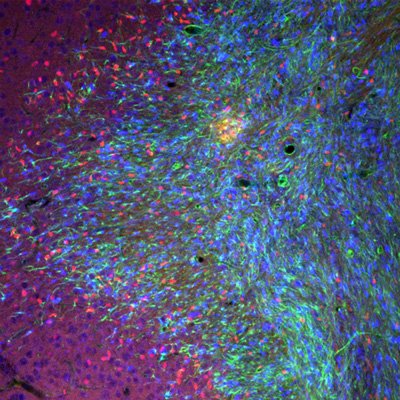
In this microscopic image, brain cells from adult mice are shown expressing the protein Olig2 (shown in red). CREDIT: Cincinnati Children’s
In laboratory tests on human cells and mouse models, an experimental therapy has been shown to stop aggressive, treatment-resistant glioblastoma and high-grade gliomas.
Testing a multi-step therapeutic strategy, the scientists, led by researchers from Cincinnati Children’s Hospital Medical Centre, found a way to use a gene therapy to shut down a gene long-implicated in the formation of high-grade gliomas called Olig2. The protein encoded by Olig2 is expressed in the majority of gliomas. Removing the Olig2 gene halts tumour growth, while elimination of Olig2-producing cells blocks tumour formation.
Drug Target Review has just announced the launch of its NEW and EXCLUSIVE report examining the evolution of AI and informatics in drug discovery and development.
In this 63 page in-depth report, experts and researchers explore the key benefits of AI and informatics processes, reveal where the challenges lie for the implementation of AI and how they see the use of these technologies streamlining workflows in the future.
Also featured are exclusive interviews with leading scientists from AstraZeneca, Auransa, PolarisQB and Chalmers University of Technology.
“We find that elimination of dividing Olig2-expressing cells blocks initiation and progression of glioma in animal models and further show that Olig2 is the molecular arbiter of genetic adaptability that makes high-grade gliomas aggressive and treatment resistant,” said Qing Richard Lu, PhD, lead investigator and scientific director of the Brain Tumour Centre at Cincinnati Children’s. “By finding a way to inhibit Olig2 in tumour forming cells, we were able to change the tumour cells’ makeup and sensitise them to targeted molecular treatment. This suggests a proof of principle for stratified therapy in distinct subtypes of malignant gliomas.”
Olig2 appears at the early stages of brain cell development. Through extensive analysis of human brain cancer cells and mouse models, the researchers observed Olig2 expression in early-stage dividing and replicating cells in tumours.
Olig2 contributes to the transformation of normal precursor cells into abnormal malignant cells that divide uncontrollably. In the context of cancer cell formation, the researchers saw Olig2 drive molecular processes that allow forming glioma cells to be highly adaptable and susceptible to the tumour-promoting effects of additional genetic changes.
Researchers then decided to eliminate Olig2-positive dividing cells during tumour formation. To use an approach more rapidly translatable from the laboratory bench to clinical bedside, they successfully tested a gene therapy that uses an engineered herpes simplex virus to deliver a suicide gene into replicating Olig2-positive cancer cells. They next administered an anti-herpes drug already in clinical use, ganciclovir (GCV). The Olig2-deleted tumours were not able to grow.
Brain cancer cells assumed astrocyte-like characteristics
Researchers also found that after Olig2 was inhibited, the forming brain cancer cells switched directions and molecular composition- going from the cells resembling oligodendrocyte precursors to assume astrocyte-like brain cell characteristics. They continued to form tumours, however these newly formed astrocyte-like brain cancer cells produce the epidermal growth factor receptor (EGFR) gene at high levels.
EGFR is a common and effective target for chemotherapy drugs used clinically to treat tumours such as breast cancers. In repeated tests in mouse models, Olig2 inhibition prompted the glioma-forming cells to transform into EGFR-expressing astrocyte-like cells. Then, in subsequent and repeated testing on the transformed human and mouse model astrocyte-like cancer cells, the researchers treated the cells with an EGFR-targeted chemotherapy drug called gefitinib. The treatment stopped the growth of new tumour cells and tumour expansion.
Dr Lu said that with additional testing, verification and refinement the experimental therapy could be especially helpful in preventing a recurrence of brain cancer in patients who have undergone an initial round of successful treatment. He added the new treatment approach would likely be used in combination with other existing therapies like radiation, surgery, other chemotherapies and targeted molecular treatments.
Related topics
Oncology
Related conditions
Glioblastoma multiforme
Related organisations
Cincinnati Children's Hospital Medical Centre



