Scientists find treatment for tumour cell population that causes tumour relapse
Posted: 10 October 2018 | Drug Target Review | No comments yet
Researchers in Europe have developed a treatment that targets a tumour cell population responsible for therapy resistance and tumour relapse, giving optimism for patients with the most frequent form of cancer.
Resistance to therapy is a major problem for cancer patients as the cells that resist therapy are the root cause of tumour relapse. A better understanding of the mechanisms associated with therapy resistance is therefore essential in order to develop better strategies to definitively eradicate cancer and prevent tumour relapse.
In a recent study, a team of researchers led by Pr. Cédric Blanpain, MD/PhD, WELBIO investigator and Professor at the Université libre de Bruxelles, Belgium identified a population of tumour cells that persist following drug treatment. These cells lead to cancer relapse after treatment has been discontinued in basal cell carcinoma, the most frequent skin cancer. The study also identified a combination of drugs that can eliminate this tumour population, thus preventing tumour relapse after treatment discontinuation.
Basal cell carcinoma is the most common human cancer, affecting several millions of new patients each year across the world. Vismodegib, a FDA-approved drug, is used for the treatment of locally advanced and metastatic basal cell carcinoma in humans. Many patients treated with vismodegib experience tumour regression during treatment, but very often their tumours relapse following treatment discontinuation.
The precise mechanisms involved in tumour regression upon Vismodegib administration and how the tumour cells resist the therapy leading to cancer relapse are poorly understood.
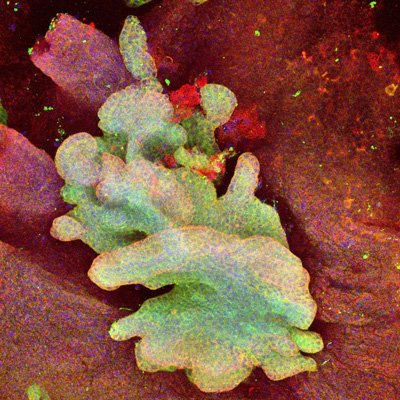
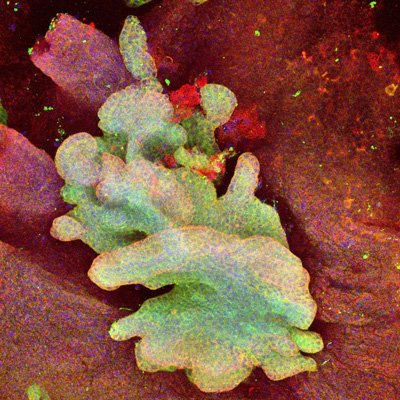
In this new study, Adriana Sánchez-Danés – Université libre de Bruxelles, ULB, Laboratory of Stem Cells and Cancer – and colleagues identified these mechanisms: They found that Vismodegib promotes the differentiation of the bulk of tumour cells, leading to their elimination. Vismodegib treatment led to the emergence of a population of dormant tumour cells characterised by active Wnt signalling that persists despite continuous drug administration.
In collaboration with the groups of Pr. Tabernero (Barcelona, Spain) and Pr. del Marmol (Brussels, Belgium), the researchers demonstrated that this population of tumour cells active for Wnt signalling was also found in patients with basal cell carcinoma treated with Vismodegib.
Adriana Sánchez-Danésand colleagues found that inhibition of Wnt signalling together with Vismodegib eliminates the persisting tumour lesions leading to tumor eradication in the vast majority of cases.
“It was really exciting to identify a combination of drugs already available in clinics that lead to the eradication of resisting tumour cells and avoiding tumour relapse in the most frequent cancer in humans”, said Adriana Sánchez-Danés, the first author of the study.
This study illustrates that Vismodegib facilitates tumour regression by promoting the differentiation of tumour cells. This demonstrates for the first time that inducing tumour differentiation is a safe and efficient strategy to treat solid tumours such as basal cell carcinoma.
“This is the first example of a FDA-approved drug used to treat solid tumour that induces tumour regression through differentiation. Tumour differentiation is an exciting route to treat cancer as it is non toxic for normal cells and was proved to be a revolutionary treatment in certain Leukaemia,” said Cédric Blanpain, the senior author of study.
“Our study also identifies a new mechanism of resistance to therapy in basal cell carcinoma and demonstrates that the administration of two existing drugs is sufficient to prevent tumour relapse in the vast majority of cases. The next step would be to conduct clinical trials using the combination of these two drugs in patients with relapsing basal cell carcinomas and possibly other cancers characterised by the activation of the two signalling pathways identified here”, finished Cédric Blanpain.
This work was supported by the FNRS, the TELEVIE, the Marian Family, the Fondation ULB, the foundation Baillet Latour, and a consolidator grant of the European Research Council.
The study was published in Nature.
Related topics
Disease research, Drug Targets, Oncology
Related conditions
Basal cell carcinoma
Related organisations
Université libre de Bruxelles (ULB)
Related people
Adriana Sánchez-Danés, Pr. Cédric Blanpain MD/PhD



